Research Article
The impact of two different doses of Dexmedetomidine to Local Anesthetic Mixture on the quality of single injection Peribulbar Block in Vitreoretinal operations

Nagat S EL-Shmaa1*, Mohamed El-Kashlan2 and Eman Ramadan Salama1
1Department of Anesthesia & Surgical ICU, Faculty of Medicine, Tanta University, Tanta, Egypt
2Magrabi Eye Hospital, Jeddah, KSA
*Address for Correspondence: Nagat S EL-Shmaa, Department of Anesthesia & Surgical ICU, Faculty of Medicine, Tanta University, Tanta, Egypt, Email: [email protected]
Dates: Submitted: 16 January 2018; Approved: 29 January 2018; Published: 30 January 2018
How to cite this article: EL-Shmaa NS, El-Kashlan M, Salama ER. The impact of two different doses of Dexmedetomidine to Local Anesthetic Mixture on the quality of single injection Peribulbar Block in Vitreoretinal operations. Int J Clin Anesth Res. 2018; 2: 001-008. DOI: 10.29328/journal.ijcar.1001005
Copyright License: © 2018 EL-Shmaa NS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Dexmedetomidine; Single injection peribulbar block; Vitreoretinal operations
Abstract
Objective: To evaluate the impact of adding two different doses of dexmedetomidine to local anesthetic mixture on the quality of single injection peribulbar block in vitreoretinal operations
Design: A prospective, double-blinded and randomized study.
Setting: carried out in operating room of our university hospital.
Patients: The study included 120 patients with viteroretinal diseases who were scheduled for vitreoretinal operations during the period from April 2016 to March 2017.
Interventions: 120 patients were randomly allocated to three groups of 40 patients each. Group I (the control group) received 5-7 ml mixture of lidocaine 2% and Levobupivacaine 0.5% with 120 IU of hyaluronidase, group II received5- 7 ml mixture of lidocaine 2% and Levobupivacaine 0.5% with 120 IU of hyaluronidase +15 µgdexmedetomidine, and group III received5- 7 ml mixture of lidocaine 2% and Levobupivacaine 0.5% with 120 IU of hyaluronidase + 30 µg dexmedetomidine
Measurements: The primary outcome was to evaluate the impact of adding two different doses of dexmedetomidine on the onset of globe anesthesia and akinesia. Secondary outcomes were the duration of globe anesthesia and akinesia, overall patient satisfaction and surgeon satisfaction.
Results: The onset of globe anesthesia was significantly shorter in group II and III in comparison with group I. Adding dexmedetomidine to the local anesthetic mixture prolonged the duration of globe analgesia, and this difference was statistically significant in group II and III in comparison with the group I.
Conclusion: Adding dexmedetomidine to a mixture of lidocaine 2% and levobupivacaine/hyaluronidase mixture in single injection peribulbar block shortened sensory and motor block onset, extended the analgesia period and the motor block duration with high patient and surgeon satisfaction.
Introduction
Regional block is the ideal anesthetic technique for ophthalmic operations since it is more safer particularly in old aged peoples who are usually risky patients and having multiple uncompensated diseases which lead to anesthetic adverse effects [1]. Moreover, regional anaesthesia is more suitable for day case surgery as it is associated with less incidence of nausea and vomiting and it attenuates endocrinal stress response related to the operation [2].
Retrobulbar block is associated with complications such as globe perforation, spread of anesthesia to the brain stem, and retrobulbar hemorrhage, so peribulbar block is considered near ideal anesthesia for eye operation because of lower tendency for major’s complication [3]. Two injection techniques with low volume are associated with optimum surgical conditions for ophthalmic operation. But, single injection is still considered safer than two injections due to increase incidence of perforations. However, it has some disadvantages as slow onset, short duration, and the need to increase volume of local anesthetic drugs that may elevate the intraocular pressure [4].
Many additives were added to local anesthetics to shorten the onset and prolong the duration of action with limited success such as hyaluronidase [5], clonidine Magnesium [6], sodium bicarbonate, and adrenaline [7]. Dexmedetomidine alpha-2 agonist, which stimulates both central and peripheral alpha-2 receptors, has been used as an additive to local anesthetics in peripheral nerve block and neuraxial anesthesia to decrease the onset and prolong the duration of analgesia [8]. The objective of the present study was to evaluate the impact of adding two different doses of dexmedetomidine to local anesthetic mixture on the quality of single injection peribulbar block in vitreoretinal operations.
Patients and Methods
This is a prospective randomized double-blinded study conducted at a university hospital and carried out on 120 patients during the period from March 2017 to December 2017 after approval by the Ethical Committee of the hospital. The CONSORT 2010 statement was used in the study.
Inclusion criteria were patients with American Society of Anesthesiologists (ASA) physical status I-II of both sexes aged between 40 and 60 years who were scheduled for vitreoretinal operations Exclusion criteria were patients who refused to enroll in the study, known allergy to studied agents, morbid obesity, history of major psychiatric disorders, coagulation disorders, chronic pain syndrome, patients with any orbital deformity, high myopes, high intraocular pressure, single eyed patients, mentally retarded patients, chronic opioids use, and current opioids treatment. Patients were informed with complete data about the techniques of analgesia and anesthesia.
All included patients were asked to take part in this study by the study participants soon after admission to the ward and a written informed consent was obtained from each patient. The surgeon and the anesthetist doing the peri-operative monitoring were blinded to the study drugs by wrapping the syringes with number codes.
Randomization was done through a computer-generated, random-number list. The random number list was performed by means of the QuickCalcs (GraphPad Software Inc., La Jolla, CA, USA). The group assigned numbers were sealed in opaque envelope and kept with the study supervisor. After the written informed consent was signed, the opaque envelope was opened to detect which drug dose would be used.
Patients were randomly allocated to three groups of 40 patients each
Group I: Group C (the control group) (n=40) received 5-7 ml mixture of lidocaine 2% and Levobupivacaine 0.5% with 120 IU of hyaluronidase according to the dimension of eye socket.
Group II:: Group D15 (n=40) received 5-7 ml mixture of lidocaine 2% and Levobupivacaine 0.5% with 120 IU of hyaluronidase +15 µg dexmedetomidine according to the dimension of eye socket.
Group III: Group D30 (n=40) received 5-7 ml mixture of lidocaine 2% and Levobupivacaine 0.5% with 120 IU of hyaluronidase + 30 µg dexmedetomidine according to the dimension of eye socket.
The local anesthetic admixture was prepared by anesthetist who was not involved in the study, so the anesthetist, the surgeon, and the patient were blinded to the type of the anesthetic admixture. All patients were fasted 6 h before the operation. No sedatives were administered to the patients. At the operation room, patients lied in supine position with nasal cannula which delivered oxygen at 3 L/min, cannula was inserted and the patients were connected to the monitor to record base line Electrocardiogram (ECG), heart rate (beats/min), systolic, diastolic blood pressure, and oxygen saturation (SpO2).
Anesthetic technique: Single peribulbar block was performed using a (25G), 16 mm bevel disposable needle. The patients lied supine and look directly ahead focusing on a fixed point on the ceiling, so that the eyes were in the neutral position. After sterilization of the lower eye lid, the globe was pushed up by the non dominant hand of the anesthetist while the needle was introduced at a point 2 mm down and medial to the inferior lacrimal canaliculus, on the inferior eyelid and the needle was advanced in an antero-posterior direction for half of its length and then obliquely towards the optical foramen according to Rizzo technique [9], until the needle became in the same plane of the bony margin of the orbit. After negative aspiration, the local anesthetic mixture was injected according to the patient’s group guarded by no overcrowding of the eye then soft intermittent digital pressure by the middle three fingers on the eye was applied for 5 min to decrease the intraocular pressure, help spread of the anesthetic solution and promote akinesia of the periorbital muscles. Time to complete the injection was considered as 0 time.
The following parameters were recorded
• Hemodynamic variables such as heart rate (beats/min), non invasive blood pressure (mmHg) and oxygen saturation were recorded just before peribulbar injection (base line), and every five minutes till the end of the surgery.
• Onset time of sensory block (in minutes) which was measured from the time of complete injection till complete loss of corneal sensation that was evaluated by gentle touching of the cornea with a cotton swab.
• Onset time and duration of globe akinesia (motor block of the eye globe) were evaluated using three point scale [10] ranged from 0 to 2 in each one of the four directions. Akinesia score is equal to the sum of the scores in the four directions ranging from 0 to 8. It was performed by asking the patient to look superior, inferior, medial and lateral every minute till 10 min. Onset of globe akinesia was calculated from the time of complete injection of the local anesthetic mixture till the complete akinesia (akinesia score 0) while the duration was calculated from the injection time till complete recovery of motor power (akinesia score 8).
• Onset and duration of lid akinesia were assessed by testing the ability of the patient to open, and to close the eye. Where 0=complete akinesia, 1=partial movement in either or both eyelid margins, 2=normal movement in either or both eyelid margins [11]. Onset of lid akinesia was measured from the time of complete injection of the local anesthetic till the occurrence of complete lid akinesia. Duration of the lid akinesia was calculated from the time of complete injection of the anesthetic solution till complete recovery from the block. A second dose (3 ml) of the local anesthetic solution may be needed if the block was incomplete after 10 min from the first injection as manifested by the full movement in any direction or ocular akinesia score ≥6. It was given at the medial canthus, where the needle passed posterior between the medial canthus and the carauncle with the bevel facing the globe. Number of patients who needed second injection was recorded in each group.
• Total volume of the local anesthetic solution which is used to obtain adequate akinesia.
• Time for adequate conditions to start the operation (corneal anesthesia plus globe akinesia score≤1 and eyelid akinesia score of 0).
• Duration of surgery.
• Surgeon satisfaction score: At the end of the procedure, the surgeon was asked to rate the ease of the procedure on a three-point scale [easy (effective block), adequate (block is incomplete but the surgeon could proceed), impossible (failed to work)] [12].
• Patient satisfaction score: it was assessed by the patient at the end of the surgery, it was as follow: 1=complete dissatisfaction, 2=some dissatisfaction, 3=complete satisfaction [13].
• Pain was assessed using the Visual Analogue Scale (VAS) where (0) represented no pain and 10 meant the worst possible pain. Postoperative rescue analgesic in form of paracetamol 30 mg/kg was given IV if VAS (4-6) or pethidine 30 mg IV if VAS >6[14].
• The time to 1st analgesic request (calculated from the time of complete injection of the local anesthetic) was recorded. The patients received intravenous ketorolac 30 mg on request.
• Sedation was measured by inverted observer assessment of alertness/sedation scale [15] in which unarousable=5 and awake=1.
• Complications of the anesthetic technique or side effects related to the test drugs were observed, recorded and treated.
At the end of the surgery, patients were transported to the post anesthesia care unit (PACU) till stable vital signs, and absence of nausea and vomiting or any side effects, then they were transported to the ward. The primary outcome was to evaluate the effect of two different doses of dexmedetomidine on the onset time of peribulbar block and the secondary outcomes were the duration and quality of peribulbar block.
Statistical Analyses
Sample size was calculated before patients’ enrollment. Based on a previous study; 36 patients in each group were required to detect a significant difference of the onset of globe akinesia of one minute at α value of 0.05 and 90% power of the study. Parametric data was presented as mean and standard deviation after analysis with one-way ANOVA test and post-hoc Test. while, categorical data was comapred by Chi-square test. The Windows version of SPSS 17 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. P value<0.05 was considered statistically significant.
Results
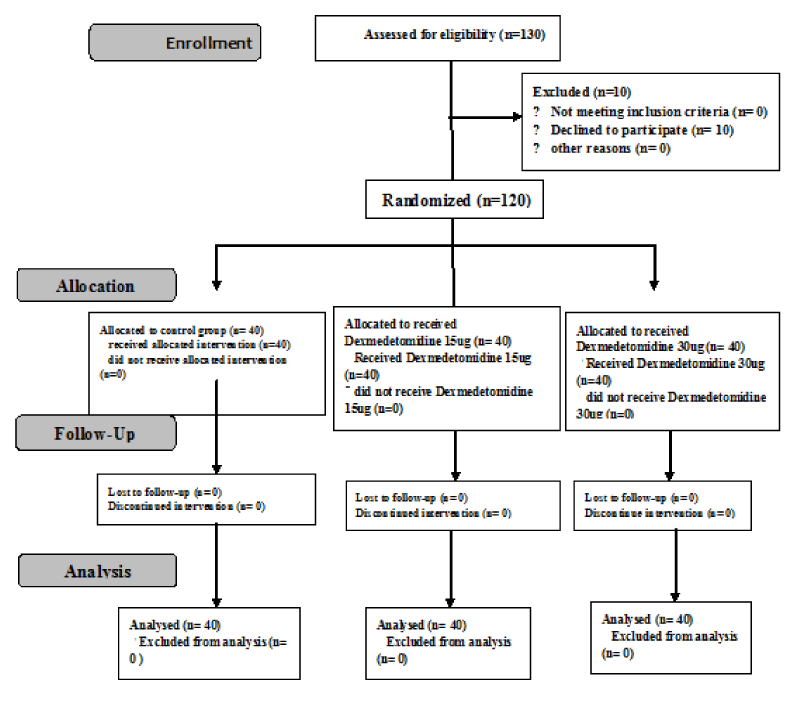
Figure 1 showed the flow chart for the study, in which 130 patients were assessed for eligibility and 120 patients were included in the study.
Figure 1: The Randomized trial flow diagram, including enrollment, intervention allocation and analysis.
Table 1 showed that the studied groups were comparable with respect to patients’ demographic data, Volume of LA (ml) and duration of surgery (P>0.05).
| Table 1: Preoperative and operative variables. | Variables | Group I (n=40) Mean±SD |
Group II (n=40) Mean±SD |
Group III (n=40) Mean±SD |
P-value | Gender distribution (male̸ female) |
13̸17 | 16̸14 | 18̸12 | 0.438 |
| ASA I̸II | 14̸16 | 13̸17 | 12̸18 | 0.877 |
| Age (years) | 57±7.4 | 56.1±5.8 | 56.6±7.2 | 0.67 |
| Weight (kg) | 75.6±6.3 | 74.4±5.6 | 76.1±6.2 | 0.62 | Volume of LA (ml) | 6.5±0.8 | 6.2±1.1 | 6.3±0.9 | 0.7 | Need for second injection | 9 (40.9%) | 3 (13.4%)* | 1 (4.5%)* | <0.001 | Duration of surgery (min) | 56.8±9.4 | 56.8±8.9 | 55.3±9.5 | 0.71 | Data are presented as mean± standard deviation or n (%). P >0.05=non-significant. P <0.01=highly significant. |
Table 2 as regards the quality of the block, it was found that adding dexmedetomidine (group II and group III) to the local anesthetic mixture significantly accelerated the onset time of sensory block in comparison to the control (group I) but without significant difference between group II and III. Onset time of globe akinesia, lid akinesia, and time for suitable conditions to start surgery were accelerated significantly in group II and group III in comparison to the control (group I) but without significant difference between group II and III. Duration of globe akinesia, and lid akinesia were significantly prolonged in group II and group III in comparison to the controls (group I) but without significant difference between group II and III. There was significant high incidence of patients who required 2nd injection in the control group in comparison togroup II and III (Table 3).
| Table 2: The quality of the peribulbar block. | Variables | Group I (n=40) Mean±SD |
Group II (n=40) Mean±SD |
Group III (n=40) Mean±SD |
P-value | Onset of sensory block (min) | 3.15±0.5 | 2.22±0.7* | 1.86±0.7* | <0.001 |
| Onset of globe akinesia (min) | 4.66±0.73 | 3.33±0.82* | 3.2±0.64* | <0.001 | Duration of globe akinesia (min) | 113.7±24.6 | 172.6±25.1* | 185.4±26.8* | <0.001 | Onset of lid akinesia (min) | 3.83±0.62 | 3.2±0.78* | 2.88±0.46* | <0.001 | Duration of lid akinesia (min) | 95.8±21.6 | 155.1±21.2* | 162.6±22.3* | <0.001 |
| Time to start surgery (min) | 9.35±1.1 | 7.35±1.33* | 6.74±1.5* | <0.001 | Data are expressed as mean±SD. P<0.05 considered significant. *Significant to control group. *Indicates statistical significance in comparison with Group I; Insignificant changes p>0.05, Significant changes p<0.05 |
Table 3 (Postoperative outcome measures): As regards the patients satisfaction, it was significantly higher in group II and group III in comparison to the control group. As regards surgeon satisfaction, it was significantly higher in group II and group III in comparison to the control group. The time to 1st analgesic request were prolonged significantly in group II and group III in comparison to the control group but without significant difference between group II and III.
| Table 3: Postoperative outcome measures. | ||||
| variables | Group I (n=40)Mean±SD | Group II (n=40) Mean±SD |
Group III (n=40) Mean±SD |
P-value |
| patient Satisfaction | 2.8±0.8 | 3.3±0.8* | 3.6±0.6* | P= 0.04 |
| surgeon Satisfaction | 2.6±0.4 | 1.4±0.3* | 1.3±0.2* | P=0.03 |
| Average postoperative VAS pain scores (0–10) | 5.1±1.3 | 2.3±0.7* | 2.5±0.7* | P<0.01 |
| Time to 1st analgesic request (min) | 157±21.3 | 239±24.6* | 245±27.1* | <0.001 |
| Data are presented as mean±standard deviation or n (%). P>0.05=non-significant. P<0.01=highly significant. |
||||
There were no recorded side effects related to the studied drug such as bradycardia, hypotension, increased intraocular tension, excessive sedation, nausea, and vomiting during the study period.
Discussion
This study was carried out to evaluate the effect of administration of two different doses of dexmedetomidine in peribulbar anesthesia and it was found that administration of either dose of dexmedetomidine to a mixture of lidocaine 2% and bupivacaine 0.5% in peribulbar block for vitreoretinal operations accelerated the onset time of sensory block, globe akinesia, lid akinesia, and time for suitable conditions to start surgery, prolonged the duration of globe akinesia, lid akinesia, and time to 1st analgesic request, and increased both patients and surgeon satisfaction without any marked side effects.
This study agrees with the results of Channabasappa et al. [16], who examined two doses of dexmedetomidine as additive to admixture of lidocaine and bupivacaine in peribulbar anesthesia and they found that administration of dexmedetomidine accelerated the onset of the peribulbar anesthesia, prolonged its duration, and duration of postoperative analgesia. Moreover, they found that the dose of 50 µg dexmedetomidine produced sedation which made the patient more cooperative. Also, this trial is in agreement with the results of Hafez et al. [17], who evaluated the effect of three doses of dexmedetomidine when added to a mixture of lidocaine 2%, bupivacaine 0.5%, and 120 IU of hyaluronidase for peribulbar anesthesia in vitreoretinal surgeries and they found that dexmedetomidine accelerated onset of sensory and motor block and increased its duration and the analgesia time. They found that the best dose was 25 µg dexmedetomidine. It also in accordance with Hala et al. [18]. Who examined the effect of adding two different doses of dexmedetomidine to levobupivacaine hyaluronidase mixture in peribulbar anesthesia and they found that dexmedetomidine accelerated onset of sensory and motor block. Abdelhamid et al. [10], compared the effect of dexmedetomidine 50 µg as an adjuvant to the local anesthetic mixture versus intravenous dexmedetomidine in their study on 90 patients scheduled for cataract surgery under peribulbar anesthesia and they,found that dexmedetomidine 50 µg as an adjuvant to the local anesthetic accelerated onset of anesthesia, and akinesia, and prolonged their duration without producing sedative effects compared to the intravenous group.
The exact mechanism by which α2-adrenergic receptor agonists produce analgesia and sedation is not fully well established. However, it can be explained by many mechanisms. Peripherally, α2-agonists decrease norepinephrine release and lead to inhibition of α2 receptor-independent action potentials. Centrally, α2-agonists inhibit substance P release in the nociceptive pathway at the level of the dorsal root neuron and activate α2 adrenoceptors [19,20].
In contrast to our results Connelly et al. [21], used clonidine (a centrally acting α2-agonist) in addition to 7 ml of 1% lidocaine and concluded that clonidine did not alter, in any appreciable way, the perioperative course for patients undergoing cataract surgery. Other studies have shown its beneficial effects in peribulbar block [22,23].
Dexmedetomidine may lead to side effects such as hypotension, bradycardia, and sedation, along with anxiolysis [20]. In our study, there were no recorded side effects related to the studied drug such as bradycardia, hypotension, increased intraocular tension, excessive sedation, nausea, and vomiting during the study period which could be explained by the use of small doses of dexmedetomidine.
Conclusion
Adding dexmedetomidine to a mixture of lidocaine 2% and levobupivacaine/hyaluronidase mixture in single injection peribulbar block shortened sensory and motor block onset, extended the analgesia period and the motor block duration with high patient and surgeon satisfaction.
Acknowledgement
The authors would like to thank the nurses at the Operation Theatre of our University Hospital, Tanta; for their assistance in conducting the study.
References
- Chishti K, Varvinskiy A. Anaesthesia for ophthalmic surgery. ATOTW. 2009; 135: 1-11.
- Godarzi M, Beyranvand S, Arbabi S, Sharoughi M, Mohtaram R, et al. Comparing the effect of using atracurium and cisatracurium as adjuvant agents to the local anesthetic substance on peribulbar-induced akinesia. Acta Med Iran. 2011; 49: 509-512.
- Loots JH, Koorts AS, Venter JA. Peribulbar anesthesia. A prospective statistical analysis of the efficacy and predictability of bupivacaine and a lignocaine bupivacaine mixture. J Cataract Surg. 1993; 19: 72-76. Ref.: https://goo.gl/ZtpSnq
- Zahl K, Jordan A, Mc Groarty J, Gotta AW. PH-adjusted bupivacaine and hyaluronidase for peribulbar block. Anesthesiology. 1990; 72: 230-232. Ref.: https://goo.gl/KvW8nv
- Baharti N, Madan R, Kaul HL, Khokhar SK, Mishra S. Effect of addition of clonidine to local anesthetic mixture for peribulbar block. Anesth Intensive Care. 2002; 30: 438-441. Ref.: https://goo.gl/6dc5Bp
- Sinha R, Sharma A, Ray BR, Chandiran R, Chandarlekha C. Effect of addition of magnesium to local anesthetics for peribulbar block: a prospective randomized double-blind study. Saudi J Anesthesia. 2016; 10: 64-67. Ref.: https://goo.gl/yK8qcx
- Reah G, Bodenham AR, Braithwaite P, Esmond J, Menage MJ. Peribulbar anesthesia using a mixture of local anaesthetic and vecuronium. Anaesthesia. 1998; 53: 551-554. Ref.: https://goo.gl/V9hS7e
- Gandhi RR, Shah AA, Patel I. Use of dexmedetomidine along with bupivacaine for brachial plexus block. Natl J Med Res. 2012; 2: 67-69. Ref.: https://goo.gl/wRBnHi
- Rizzo L, Marini M, Rosati C, Calamai I, Nesi M, et al. Peribulbar anesthesia: a percutaneous single injection technique with a small volume of anesthetic. Anesthesia & Analgesia. 2005; 100: 94-96. Ref.: https://goo.gl/ktEZ3p
- Abdelhamid AM, Mahmoud AAA, Abdelhaq MM, Yasin HM, Bayoumi ASM. Dexmedetomidine as an additive to local anesthetics compared with intravenous dexmedetomidine in peribulbar block for cataract surgery. Saudi Anesthesia. 2016; 10: 50-54. Ref.: https://goo.gl/FbVmKP
- Sarvela PJ. Comparison of regional ophthalmic anesthesia produced by pH adjusted 0.75% and 0.5% bupivacaine and 1% and 1.5% etidocaine, all with hyaluronidase. Anesthesia & Analgesia. 1993; 77: 131-134. Ref.: https://goo.gl/PVd2d6
- Ringland R, Early S. Conscious sedation: documenting the procedure. J Emerg Nurs. 1997; 23: 611-617. Ref.: https://goo.gl/tNoQhR
- Wang F, Shen X, Guo X, Peng Y, Gu X, et al. Epidural analgesia in the latent phase of labor and the risk of cesarean delivery: a five-year randomized controlled trial. Anesthesiology. 2009; 111: 871-880. Ref.: http://bit.ly/2WIDYIg
- EL-Shmaa NS, El-Baradey GF. The Efficacy of Etomidate-Fentanyl versus Dexmedetomidine-Ketamine for Procedural Sedation and Analgesia during Upper Endoscopy and Biopsy: A Prospective, Randomized Study. J Anesth Clin Res. 2014; 5: 1-5. Ref.: http://bit.ly/2KfvVw0
- Hall JE, Uhrich TD, Barney JA, Arian SR, Ebert TJ. Sedation, amnesic and analgesic properties of small dose dexmedetomidine infusion. Anesthesia & Analgesia. 2000; 90: 699-705. Ref.: https://goo.gl/oDynE6
- Channabasappa SM, Shetty VR, Dharmappa SK, Sarma J. Efficacy and safety of dexmedetomidine as an additive to local anesthetics in peribulbr block for cataract surgery. Anesth Essays Res. 2013; 7: 39-43. Ref.: http://bit.ly/2KOmYZR
- Hafez M, Fahim MR, Abdelhamid MH, Youssef MMI, Salem AS. The effect of adding dexmedetomidine to local anesthetic mixture for peribulbar block in vitreoretinal surgeries. Egyptian J Anesthesia. 2016; 32: 573-579. Ref.: https://goo.gl/iJXAU3
- El-Ozairy Hala S, Tharwat AI. Comparative study of the effect of adding two different doses of dexmedetomidine to levobupivacaine/hyaluronidase mixture on the peribulbar block in vitreoretinal surgery. Ain-Shams J Anesthesiol. 2014; 7: 393-399. Ref.: https://goo.gl/5FhgqP
- Eisenach JC, De Kock M, Klimscha W. Alpha (2)-adrenergic agonists for regional anesthesia. A clinical review of clonidine (1984-1995). Anesthesiology. 1996; 85: 655-674.
- Guo TZ, Jiang JY, Buttermann AE, Maze M. Dexmedetomidine injection into the locus ceruleus produces antinociception. Anesthesiology. 1996; 84: 873-881.
- Connelly NR, Camerlenghi G, Bilodeau M, Hall S, Reuben SS, et al. Use of clonidine as a component of the peribulbar block in patients undergoing cataract surgery. Regional Anesthesia and Pain Medicine. 1999; 24: 426-429. Ref.: https://goo.gl/tpFJPT
- Madan R, Bharti N, Shende D, Khokhar SK, Kaul HL. A dose response study of clonidine with local anesthetic mixture for peribulbar block: a comparison of three doses. Anesthesia & Analgesia. 2001; 93: 1593-1597. Ref.: https://goo.gl/dyqhoS
- Bahy-Eldeen HM, Faheem MR, Sameer D, Shouman A. Use of clonidine in peribulbar block in patients undergoing cataract surgery. Aust J Basic Appl Sci. 2011; 5: 247-250. Ref.: http://bit.ly/2KMoJXv