More Information
Submitted: August 21, 2023 | Approved: August 29, 2023 | Published: August 30, 2023
How to cite this article: Thomas G. Deciphering the Rosetta Stone - Trans-Mitral Doppler Patterns for a Simplified Study of Left Ventricular Systolic Dysfunction. Int J Clin Anesth Res. 2023; 7: 008-011.
DOI: 10.29328/journal.ijcar.1001023
Copyright License: © 2023 Thomas G. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Trans-mitral Doppler; Diastolic dysfunction; Diastology; Systolic dysfunction; Systology
Deciphering the Rosetta Stone - Trans-Mitral Doppler Patterns for a Simplified Study of Left Ventricular Systolic Dysfunction
George Thomas*
Department of Cardiology, Saraf Hospital, Sreekandath Road, Kochi 682016, India
*Address for Correspondence: George Thomas, MD, FCSI, FIAE, Department of Cardiology, Saraf Hospital, Sreekandath Road, Kochi 682016, India, Email: [email protected]
There is a renewed interest in heart failure treatments. With this, there is an increasing interest in heart failure with preserved ejection fraction. Trans-mitral Doppler is commonly used in the assessment of ‘diastolic’ function. It is fashionable to discuss diastolic dysfunction and diastology with the result that the more important systolic dysfunction has become passé. The current literature equates trans-mitral Doppler patterns to diastolic function when actually it is more relevant in systolic dysfunction. This article is an attempt to correct this flawed perception of trans-mitral Doppler.
There is a renewed interest in heart failure treatments [1]. Newer therapeutic options are popping up with increased frequency. The concept of “backward failure” was introduced in 1947 [2]. Later this was described as “diastolic heart failure”. The same is now called heart failure with preserved ejection fraction (HFpEF). With this “diastology” has become more fashionable and heart failure with reduced ejection fraction (HFrEF) is being relegated to the background [3,4]. However, the heart being a pump, the evaluation of systolic function is crucial. There are several complicated methods to evaluate systolic dysfunction [5]. In such a scenario it is of utmost importance to have a simple assessment of the systolic function. The study of trans-mitral flow is an easy way to assess systolic function too. It can be undertaken using the simplest machines without using sophisticated techniques and calculations. A detailed methodology of a simplified study of trans-mitral Doppler patterns has been described earlier [6].
Just what do you mean by diastolic dysfunction?
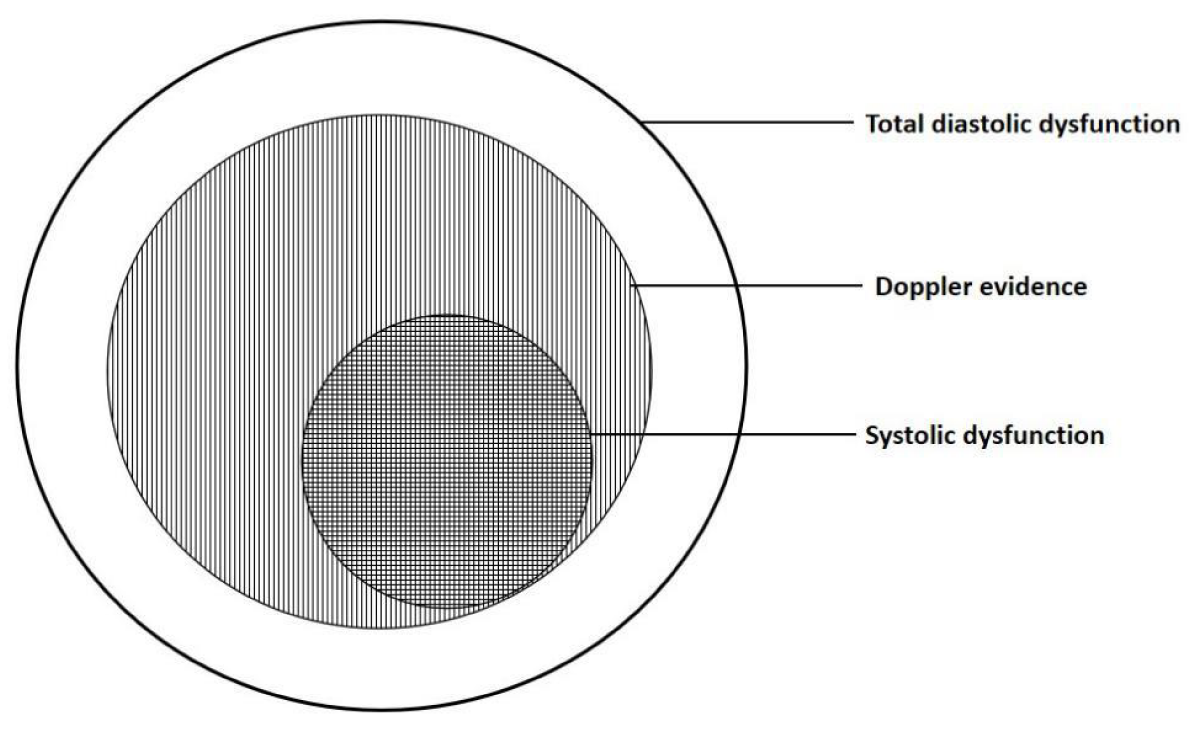
Diastole and systole are two sides of the same coin and are not mutually exclusive (Figure 1). Abnormalities that occur during the diastolic part of the cardiac cycle would be diastolic dysfunction. Thus, ‘diastolic dysfunction’ will cover the universal set of all diastolic abnormalities in the heart. This will include components like left ventricular, right ventricular, left atrial, right atrial, mitral valve, tricuspid valve, aortic valve, pulmonary valve, aortic root, pulmonary artery, pericardial, and rhythm-related diastolic abnormalities. Most commonly we address left ventricular diastolic dysfunction. In current literature, diastolic dysfunction usually means left ventricular diastolic dysfunction and its attendant pressure and Doppler abnormalities.
Figure 1: Schematic diagram of cardiac dysfunction. Cardiac dysfunction starts with diastolic dysfunction. The clear area shows cardiac dysfunction without Doppler abnormalities. Doppler evidence is shown as the vertical hatched area. This also includes systolic dysfunction shown as the horizontal hatched area. This overlaps the vertical hatched area. Thus Doppler evaluation is more specific for systolic dysfunction.
Doppler echocardiography has made it easy to evaluate “diastolic function” by the analysis of trans-mitral flow. In the process, we have given undue importance to “diastology” in general and “diastolic dysfunction” in particular [7,8]. But what do you mean by diastolic dysfunction?
The earliest changes in cardiac dysfunction occur at the molecular, cellular, and structural levels [9]. Doppler abnormalities set in later. When we say diastolic dysfunction do we mean molecular/cellular abnormalities, abnormal chamber properties, abnormal pressures, abnormal Doppler patterns, or diastolic heart failure? Most literature equates abnormal Doppler patterns with diastolic dysfunction [9,10].
Diastole is a sensitive part of the cardiac cycle. The earliest abnormality in any cardiac pathology is diastolic dysfunction. So it is but natural that any cardiac disease can cause LV diastolic dysfunction to variable extents. Doppler can only detect ‘diastolic dysfunction’ at later stages. Abnormal Doppler Filling Patterns (DFP) are only a part of the total diastolic dysfunction set. So being a ubiquitous entity, the absence of abnormal DFP need not mean the absence of diastolic dysfunction. LV diastolic dysfunction can occur in very mild forms and regional forms, which may not be evident on Doppler assessment. Similarly, the mere presence of abnormal DFP need not mean the presence of HFpEF. So using the vague term ‘diastolic dysfunction’ is meaningless.
The problems with the present approach to trans-mitral Doppler are:
1. Abnormal trans-mitral Doppler patterns are considered to indicate diastolic dysfunction exclusively.
2. There is no differentiation between Doppler patterns of normal and impaired systolic function.
3. The progression of “diastolic dysfunction” (from mild to severe) is assumed to occur in all situations.
The practical issues with the above problems are:
If E-A reversal (Grade 1) is mild, pseudonormal (Grade 2) is moderate and restrictive (Grade 3) is severe diastolic dysfunction,
1. Does it mean that restrictive cardiomyopathy is severe diastolic dysfunction?
2. Does hypertension with initial E-A reversal become restrictive cardiomyopathy as the disease progresses?
3. In systolic dysfunction does the restrictive pattern indicate severe diastolic dysfunction?
Many such oddities are possible with the current approach. This means that there is a need to approach transmitral Doppler patterns in a more realistic and rational manner.
Trans-mitral Doppler for the assessment of cardiac function
Doppler should be seen as a tool to assess global cardiac function - both diastolic and systolic. Trans-mitral Doppler is to study left ventricular function. It is important to note that this is a ‘dual use’ tool - like a measuring tape which can measure chest expansion or abdominal girth depending on where it is applied. Here the term to be used is Doppler Filling Patterns (DFP) instead of Doppler diastolic patterns so as to include the study of systolic function. The term Doppler diastolic patterns gives the impression that trans-mitral Doppler is exclusively used to study diastolic function [11].
Thus trans-mitral Doppler can be used to assess systolic and diastolic functions depending on the clinical situation. It is like measuring the abdominal girth for metabolic syndrome. Metabolic syndrome is a common entity. In a female, the implication of the abdominal girth depends on whether the patient is pregnant. Thus the same girth measurement would mean say ‘severe metabolic syndrome’ or ‘advanced pregnancy’. In this case, the implication of ‘advanced pregnancy’ is clinically more relevant. Thus ‘severe diastolic dysfunction in systolic dysfunction’ is an oxymoron. It is like labeling a case of advanced pregnancy as ‘severe metabolic syndrome in pregnancy’. So in the case of Doppler patterns, these should be analyzed in the context of systolic function. If the systolic function is impaired, it is an assessment of the severity of systolic dysfunction.
Trans-mitral Doppler for systolic function
Traditionally trans-mitral Doppler is equated with diastolic function [12]. However diastolic indices are used for systolic function. Classical cardiology tells us that end-diastolic pressure, end-diastolic volume, etc. reflect systolic function. Left ventricular end-diastolic pressure (LVEDP) is the gold standard for systolic function. Other diastolic indices indicating systolic function are E-point septal separation and B-bump [13] Diastole is a distinct and important physiological entity. But systole is an important clinical entity. Since diastolic indices reflect systolic properties, the filling patterns that occur in diastole are more relevant for systolic function.
Which brings us to the most important question. What significant information do trans-mitral Doppler patterns provide? Does it tell us more about diastolic function or systolic function?
As mentioned earlier, diastolic dysfunction is a vague entity. It is a reality but pursuing it in clinical practice with Doppler is fraught with problems. The heart is a pump, and the systolic function is critical. It is important to detect systolic dysfunction at any cost. Transmitral Doppler shows a good relation with systolic dysfunction [14]. The progression or regression of patterns is consistent with improvement or deterioration. So these ‘diastolic’ patterns are more relevant for systolic dysfunction.
Systology
If the study of diastolic function is ‘diastology’, then the study of systolic function is ‘systology’. Systolic dysfunction is usually associated with increased LV end-diastolic pressure and left atrial pressure. This can be studied by LV DFP. Basic echocardiography tells us that a brisk and well-opening mitral valve signifies good systolic function. Thus diastolic phenomena are indicators of systolic function. Patients with progressively more abnormal diastolic patterns have greater structural abnormalities with larger left atrial and LV size and lower LV ejection fractions [15]. So, in cases with impaired systolic function, LV DFP can be used to assess the severity of impairment and prognosis. In such cases, trans-mitral Doppler shows continuous pattern changes (hierarchy of patterns) depending on the severity of systolic dysfunction. By impaired systolic function, we could also include cases with wall motion abnormalities with apparently normal ejection fraction and apparently normal overall LV contractility. If Pattern 0 is normal, Pattern 1 showing a small E wave and a large A wave could indicate mild systolic dysfunction. Pattern 2, showing a ‘pseudo-normalization’ pattern denoted by an apparently normal E and A wave could indicate moderate impairment. Finally, pattern 3 with a very prominent E wave and a minuscule A wave could indicate severe hemodynamic impairment and is associated with the worst prognosis. In cases of systolic dysfunction, the LV DFP is a continuous variable reflecting the increasing left atrial pressures which proceed to atrial failure in pattern 3. As a rule of thumb patterns 0 - 1 signifies a pressure of about 12 - 15 mmHg, patterns 1 - 2 about 15 - 18 mmHg, patterns 2 - 3 about 18 - 20 mmHg, and pattern 3+ greater than 20 mmHg. These pressure values are only indicative. The pattern recognition and its changes are best in the same patient with a reasonably maintained heart rate. With this approach the absolute velocity values become irrelevant. The relative E and A magnitudes will allow pattern recognition. The increasing left atrial pressure could be confirmed by the pulmonary venous flow abnormalities in ideal conditions. As a corollary, in cases with resting or stress-induced wall motion abnormalities and apparently normal ejection fraction, a pattern to the right of 0 could indicate a mild systolic dysfunction. In serial studies of chronic cases, a shift to the right could indicate worsening systolic function while a shift to the left could indicate improvement.
Trans-mitral Doppler should not be interpreted in isolation. It is important to know the systolic function. There are several methodologies and indices for evaluating systolic function but ejection fraction is the most commonly used parameter. As there are many pitfalls in echocardiographic ejection fraction estimation, we rely on eyeball estimation in this simplified methodology [16,17]. However good experience is needed for reliable eyeball evaluation of systolic function. Artificial Intelligence may be helpful in such situations [18].
Here the algorithm runs like this: Ask the following questions: Is the systolic function impaired? The answer could be Yes, No, or Doubtful. When in doubt, consider the systolic function as mildly impaired. Next, are there regional wall motion abnormalities? The answer could be Yes, No, or Doubtful. If yes, is it compensated by the other segments? When in doubt consider wall motion abnormality as present depending on the clinical circumstances. Usually, a wall motion abnormality indicates impaired systolic function. However, the global systolic function could be compensated by the other segments. Global hypokinesia is also easily detectable by eyeball examination.
Thus instead of invoking diastolic dysfunction for all abnormal trans-mitral Doppler patterns, we must identify them as severity of systolic dysfunction if the systolic function is impaired. However, if the systolic function is normal it would point to pure diastolic dysfunction [19]. With such an approach, many of the cases of diastolic heart failure will turn out to be systolic failure. By following this schema we can unravel some of the mysteries of the Rosetta Stone of Doppler’s “diastology” by factoring in systolic dysfunction [20,21].
- Murphy SP, Ibrahim NE, Januzzi JL Jr. Heart Failure With Reduced Ejection Fraction: A Review. JAMA. 2020 Aug 4;324(5):488-504. doi: 10.1001/jama.2020.10262. Erratum in: JAMA. 2020 Nov 24;324(20):2107. PMID: 32749493.
- Heyer HE, Harrison TR. The backward failure theory of congestive heart disease. Mod Concepts Cardiovasc Dis. 1947 Nov;16(11):1-4. PMID: 18856413.
- Nagueh SF. Diastology: 2020-A practical guide. Echocardiography. 2020 Nov;37(11):1919-1925. doi: 10.1111/echo.14742. Epub 2020 Jun 1. PMID: 32476157.
- Vasan RS, Xanthakis V, Lyass A, Andersson C, Tsao C, Cheng S, Aragam J, Benjamin EJ, Larson MG. Epidemiology of Left Ventricular Systolic Dysfunction and Heart Failure in the Framingham Study: An Echocardiographic Study Over 3 Decades. JACC Cardiovasc Imaging. 2018 Jan;11(1):1-11. doi: 10.1016/j.jcmg.2017.08.007. Epub 2017 Oct 5. PMID: 28917679; PMCID: PMC5756128.
- Chengode S. Left ventricular global systolic function assessment by echocardiography. Ann Card Anaesth. 2016 Oct;19(Supplement):S26-S34. doi: 10.4103/0971-9784.192617. PMID: 27762246; PMCID: PMC5100240.
- Thomas G. A simplified study of trans-mitral Doppler patterns. Cardiovasc Ultrasound. 2008 Nov 28;6:59. doi: 10.1186/1476-7120-6-59. PMID: 19040751; PMCID: PMC2607254.
- Lester SJ, Tajik AJ, Nishimura RA, Oh JK, Khandheria BK, Seward JB. Unlocking the mysteries of diastolic function: deciphering the Rosetta Stone 10 years later. J Am Coll Cardiol. 2008 Feb 19;51(7):679-89. doi: 10.1016/j.jacc.2007.09.061. PMID: 18279730.
- Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016 Apr;29(4):277-314. doi: 10.1016/j.echo.2016.01.011. PMID: 27037982.
- Silbiger JJ. Pathophysiology and Echocardiographic Diagnosis of Left Ventricular Diastolic Dysfunction. J Am Soc Echocardiogr. 2019 Feb;32(2):216-232.e2. doi: 10.1016/j.echo.2018.11.011. PMID: 30717860.
- Palatini P, Frigo G, Vriz O, Bertolo O, Dal Follo M, Daniele L, Visentin P, Pessina AC; HARVEST Study Group. Early signs of cardiac involvement in hypertension. Am Heart J. 2001 Dec;142(6):1016-23. doi: 10.1067/mhj.2001.119378. PMID: 11717606.
- Lewis BS. Doppler diastolic transmitral ventricular filling patterns--towards a better understanding. Eur Heart J. 1996 Apr;17(4):493-5. doi: 10.1093/oxfordjournals.eurheartj.a014897. PMID: 8733077.
- Stoddard MF, Labovitz AJ, Pearson AC. The role of Doppler echocardiography in the assessment of left ventricular diastolic function. Echocardiography. 1992 Jul;9(4):387-406. doi: 10.1111/j.1540-8175.1992.tb00483.x. PMID: 10147786.
- Araujo AQ, Araujo AQ. Elucidating the B bump on the mitral valve M-mode echogram in patients with severe left ventricular systolic dysfunction. Int J Cardiol. 2004 May;95(1):7-12. doi: 10.1016/j.ijcard.2003.02.003. PMID: 15159031.
- Previtali M, Chieffo E, Ferrario M, Klersy C. Echocardiographic evaluation of left ventricular diastolic function: correlation between echocardiographic and hemodynamic parameters. Minerva Cardioangiol. 2007 Dec;55(6):733-40. PMID: 18091642.
- Yamada H, Goh PP, Sun JP, Odabashian J, Garcia MJ, Thomas JD, Klein AL. Prevalence of left ventricular diastolic dysfunction by Doppler echocardiography: clinical application of the Canadian consensus guidelines. J Am Soc Echocardiogr. 2002 Oct;15(10 Pt 2):1238-44. doi: 10.1067/mje.2002.124877. PMID: 12411911.
- Cikes M, Solomon SD. Beyond ejection fraction: an integrative approach for assessment of cardiac structure and function in heart failure. Eur Heart J. 2016 Jun 1;37(21):1642-50. doi: 10.1093/eurheartj/ehv510. Epub 2015 Sep 28. PMID: 26417058.
- Unlüer EE, Karagöz A, Akoğlu H, Bayata S. Visual estimation of bedside echocardiographic ejection fraction by emergency physicians. West J Emerg Med. 2014 Mar;15(2):221-6. doi: 10.5811/westjem.2013.9.16185. PMID: 24672616; PMCID: PMC3966449.
- Barry T, Farina JM, Chao CJ, Ayoub C, Jeong J, Patel BN, Banerjee I, Arsanjani R. The Role of Artificial Intelligence in Echocardiography. J Imaging. 2023 Feb 20;9(2):50. doi: 10.3390/jimaging9020050. PMID: 36826969; PMCID: PMC9962859.
- Thomas G. Classification of transmitral Doppler patterns. Indian Heart J. 2005 May-Jun;57(3):275-6. PMID: 16196192.
- Nishimura RA, Tajik AJ. Evaluation of diastolic filling of left ventricle in health and disease: Doppler echocardiography is the clinician's Rosetta Stone. J Am Coll Cardiol. 1997 Jul;30(1):8-18. doi: 10.1016/s0735-1097(97)00144-7. PMID: 9207615.
- Saha SK, Kiotsekoglou A, Nanda NC. Echocardiography 2020: Toward deciphering the "Rosetta stone" of left ventricular diastolic function. Echocardiography. 2020 Nov;37(11):1886-1889. doi: 10.1111/echo.14830. PMID: 33283344.