More Information
Submitted: December 03, 2022| Approved: December 16, 2022 | Published: December 19, 2022
How to cite this article: Agarwal S, Bansal S. To evaluate the stress response to tracheal intubation by macintosh laryngoscope and intubating laryngeal mask airway. Int J Clin Anesth Res. 2022; 6: 007-013.
DOI: 10.29328/journal.ijcar.1001020
Copyright License: © 2022 Agarwal S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hemodynamic parameters; Intubating laryngeal mask airway; Macintosh laryngoscope
To evaluate the stress response to tracheal intubation by macintosh laryngoscope and intubating laryngeal mask airway
Somika Agarwal* and Sapna Bansal
and Sapna Bansal
Department of Anaesthesiology, Maharishi Markandeshwar University, Mullana, Haryana, India
*Address for Correspondence: Somika Agarwal, MD Anesthesia, Department of Anaesthesiology, Maharishi Markandeshwar University, Mullana, Haryana, India, Email: [email protected]
Aim: To evaluate the hemodynamic changes and side effects during endotracheal intubation with Macintosh laryngoscope and intubating laryngeal mask airway.
Materials and methods: A prospective, simple randomized, comparative study on 100 patients 18 years - 60 years of age, divided into two groups: Group A comprising intubation with Macintosh laryngoscope and Group B intubation through ILMA.
Results: Total intubation time (in seconds) of group A was 24.38 + 3.26 seconds and of the group, B was 42.94 + 1.24 seconds. At 2,4 and 6, a higher rise in mean heart rate was noted in group A (p < 0.05). At 2,4,6 and 8 minutes difference in mean SBP and mean DBP of the two groups was statistically significant with a p - value of < 0.05 with a significant increase of mean SBP and mean DBP in patients of group A. The difference for all complications was not significant between the two groups.
Conclusion: Intubation via intubating laryngeal mask airway can be done as an alternative to direct laryngoscopy using a Macintosh blade as intubation via intubating laryngeal mask airway has shown to have lesser hemodynamic changes.
Management of the airway at the time of general anesthesia has always been a matter of utmost accountability and liability of an anesthetist as instances of hypoxic brain injury or even death may occur within a few minutes in absence of airway patency. Recently in this century, new techniques and instruments have come into the trend for tracheal intubation which has made general anesthesia more efficient and safer.
During anesthesia, patients tend to lose their coughing reflex (a protective airway reflex), patency of the airway, and normal breathing pattern occasionally due to the effects of anesthetic drugs used. For the maintenance of an open airway and regulation of the breathing pattern, an endotracheal tube is inserted in the trachea after the patient is induced with general anesthetic agents. The endotracheal tube is mostly preferred for maintaining the airway but alternative devices like laryngeal mask airways and face masks can also assist respiration and maintain the airway.
General anesthesia induction by intubation via direct laryngoscope is known to cause a stress response [1]. Many factors are responsible for such a response. Pharyngeal structures get stimulated due to the insertion of the laryngoscopic blade and distension of supraglottic tissue takes place leading to stimulation of sympathetic activity, which brings about certain hemodynamic changes in a patient [2,3]. Various changes that can be seen are tachycardia, hypertension, and cardiac arrhythmias. These changes may not lead to any serious complications in a patient who has no other underlying comorbidity. But in a patient who has a pre-existing cardiovascular or respiratory or cerebral disease, these changes can cause serious complications such as pulmonary edema, myocardial infarction, and cerebrovascular hemorrhage [4-6]. Thus, these responses need to be attenuated by either using other airway management techniques.
Supraglottic airway/extragalactic airway devices have been used to aid endotracheal intubation and have been advantageous over direct laryngoscopy.
They can be inserted blindly into the pharynx and can ascertain a patent pathway for ventilation, oxygenation, and delivering anesthetic inhalational agents and all of these can be achieved without the need for tracheal intubation.
In 1977, Dr. Archie Brain first described the intubating LMA (ILMA). They are specially designed to allow blind intubation that doesn’t cause any trauma to the airway structures. To prevent encroachment on the larynx, the tip of the tube is soft and molded and the tube itself is made straight and wire-reinforced [7,8].
The mask of the ILMA that is cuffed sits on top of the glottis therefore, there is no distortion of the extra glottis structures which ultimately results in less laryngeal stimulation causing the stress response to be lesser [9]. Although there are a few disadvantages of the ILMA as well like: there is an increased risk of gastrointestinal aspiration, the airway being less secure, there is a greater risk of a gas leak, etc., even then it outdates intubation via direct laryngoscope due to the fact that it helps lessen the hemodynamic changes.
Thus, this study aims to evaluate the degree and extent of these hemodynamic changes both during intubation via direct laryngoscopy with a macintosh blade and via ILMA.
Objectives
To observe the number of attempts required and total time taken for insertion of the endotracheal tube with macintosh laryngoscope and with ILMA. A secondary objective was to assess the HR, SBP, DBP, MAP and SpO2 in patients undergoing intubation via Macintosh blade and ILMA at stipulated time intervals (before intubation and at every 2 minutes interval till 10 minutes post-intubation) and post-intubation complications.
The study was carried out in 100 patients of either gender aged between 18 to 60 years, of ASA and Mallampatti (MP) grade I and II at Maharishi Markandeshwar University undergoing elective surgery under general anesthesia requiring endotracheal intubation with controlled venti-lation, after the approval from the Ethical committee of the institution.
Allocation of groups:
The patients were divided randomly by computer-generated numbers into two groups with 50 patients in each group.
Group A (n = 50): Endotracheal intubation with Macintosh laryngoscope
Group B (n = 50): Endotracheal intubation through ILMA
Study design: A prospective, simple randomized comparative study.
Inclusion criteria
1. BMI2
2. MP grading I and II
3. No history of difficult intubation
4. Elective surgeries
5. Mouth opening >/= 4 cm
Exclusion criteria
1. BMI > 30 kg/m2
2. MP grading III and IV
3. Patient with a history of difficult intubation.
4. Pregnant females.
5. Emergency surgeries.
6. Mouth opening less than 4 cm.
7. Head and neck surgical procedures
A post hoc power analysis was conducted using the software package, G*Power version 3.1.9.2 (Franz Faul, University Kiel, Germany). The sample size was estimated from the results of the previous study18 using the Intubation time as the parameter, which is the primary outcome of our study. Our sample size came out to be 50 subjects per group at a power of 0.99 and with an effect size of 1.67 with a 10% chance of error with α = 0.05, β = 0.20 and a confidence interval of 95%.
Pre-anesthetic evaluation of the patient was done an evening prior to the surgery. Written informed consent was taken from the patient. Patients were kept fasting for six hours for solids.
In the preoperative room patient’s vital parameters were checked. An Intravenous (IV) line was secured with an 18 G cannula and NS or RL (ringer lactate) 500 ml was started, baseline parameters like blood pressure, peripheral oxygen saturation, and heart rate were recorded.
The patient was then assigned to one of the two groups (intubation via DL and intubation via ILMA) randomly.
Inside the operating room, SBP, DBP, MAP and HR will be recorded prior to induction. The patient was preoxygenated for 3 minutes and iv midazolam (0.05 mg/kg) and iv glycopyrrolate (0.005 mg/kg) were used as premedication agents. An appropriate laryngoscope macintosh blade was selected on the basis of the body size of each patient in group A (DL), as well as in group B (ILMA). Correct placement of the tube was assured by checking bilateral airway entry.
Anesthesia was maintained in both groups with 50% oxygen in the air and 1% isoflurane and top-up doses of muscle relaxant when needed. Controlled mechanical ventilation of the lung was adjusted for the maintenance of EtCO2 in the range of 30 mmHg - 35 mmHg as measured by capnography. No. of attempts for endotracheal intubation were noted. More than 3 no. of attempts were considered as failed intubation. Time of insertion was observed from the point of insertion of the direct laryngoscope in group A and ILMA in group B respectively till confirmation of placement of ETT by capnography. Hemodynamic parameters such as heart rate, systolic and diastolic blood pressure, mean arterial pressure and oxygen saturation was noted at various time intervals like before intubation, 2 mins, 4 mins, 6 mins, 8 mins and 10 mins post-intubation. Any associated complications such as trauma, bronchospasm, laryngospasm, cough, or sore throat were recorded post-extubation.
Statistical analysis
Statistical analysis was done for all quantitative variables of each group. Data was described in terms of range; mean ± standard deviation (± SD), frequencies (number of cases) and relative frequencies (percentages) as appropriate. All variables at baseline, pre-intubation, 2,4,6,8 and 10 minutes post-intubation were presented as mean with SD. Patient characteristics were compared with unpaired Student’s t-test. Rates of HR, SBP, DBP, MAP and SpO2 were analyzed with analysis of variance test. For comparing categorical data, Chi-square (X2) test was performed. A probability value (p - value) less than 0.05 was considered statistically significant.
The present study was carried out in the department of Anaesthesiology on 100 patients from the time period of August 2018 to March 2020. The data thus obtained was analyzed and the observations made were summarized.
The mean age of groups A and B was 38.16 + 12.11 and 35.76 + 14.01 years respectively. The difference between the two means was not statistically significant. Observations reflected no significant difference in sex distribution in both groups. The mean BMI of group A was observed as 24.57 + 2.26 kg/m2 and the mean BMI of group II was 24.42 + 1.72 kg/m2 with no significant difference between the two groups. No significant difference was noted in ASA grading between the two groups (Table 1).
| Table 1: Demographic data (mean ± SD or number of patients). | ||
| Variables | Laryngoscope group (n = 50) | Ilma group (n = 50) |
| Age (years) | 38.16 + 12.11 | 35.76 + 14.01 |
| Sex ratio (m:f) | 19:31 | 25:25 |
| BMI (kg/m2) | 24.57 + 2.26 | 24.42 + 1.72 |
| ASA status | 28:22 | 25:25 |
Both groups were comparable in terms of Mallampatti grading, thyromental distance, mouth opening and breath-holding time with a non-significant p - value.
Variables considered in hemodynamics were heart rate, systolic blood pressure, diastolic pressure, mean blood pressure and Sp02. All the hemodynamic parameters were compared among both the groups at T0, T1, T2, T3, T4 and T5 time intervals.
In our study number of patients who had successful intubation on the first attempt was 40 (80%) and 42 (84%) in group A and group B respectively with a non-significant p - value of 0.603. The total intubation time (in seconds) of group A was 24.38 + 3.26 seconds and of the group, B was 42.94 + 1.24 seconds. The difference between the two means was statistically significant with more insertion time taken in group B subjects (Table 2).
| Table 2: Intubation data [mean ± SD or number (%) of patients]. | ||
| Variables | Laryngoscope group (n = 50) | Ilma group (n = 50) |
| Intubation time (seconds)* | 24.38 + 3.26 | 42.94 + 1.24 |
| Number of attempts - ONE | 40 | 42 |
| Number of attempts - TWO | 10 | 8 |
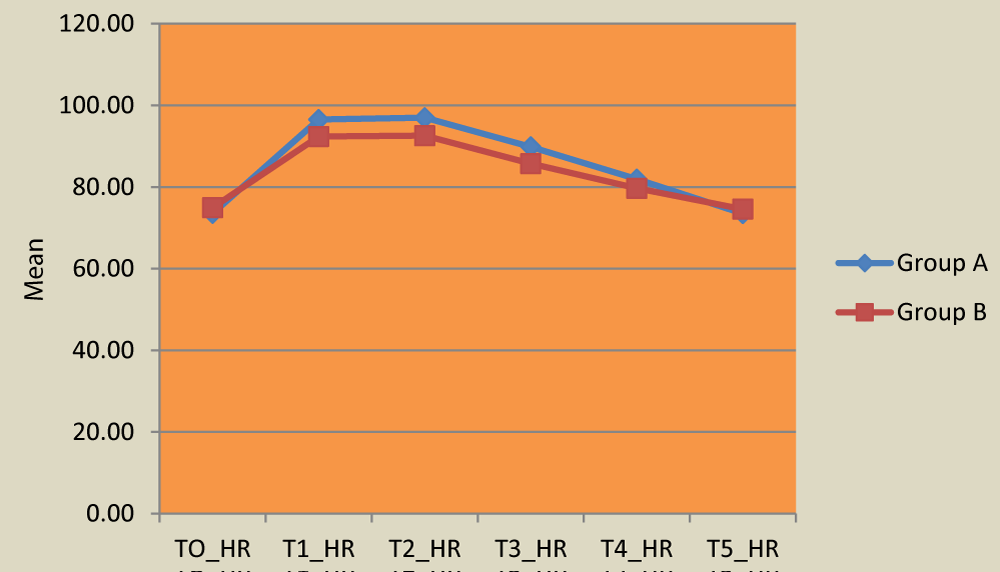
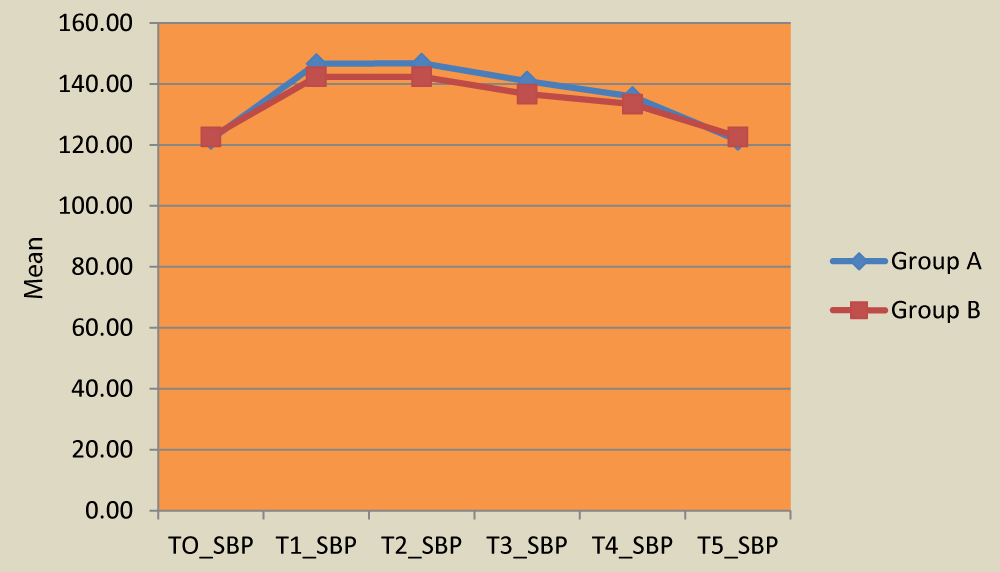
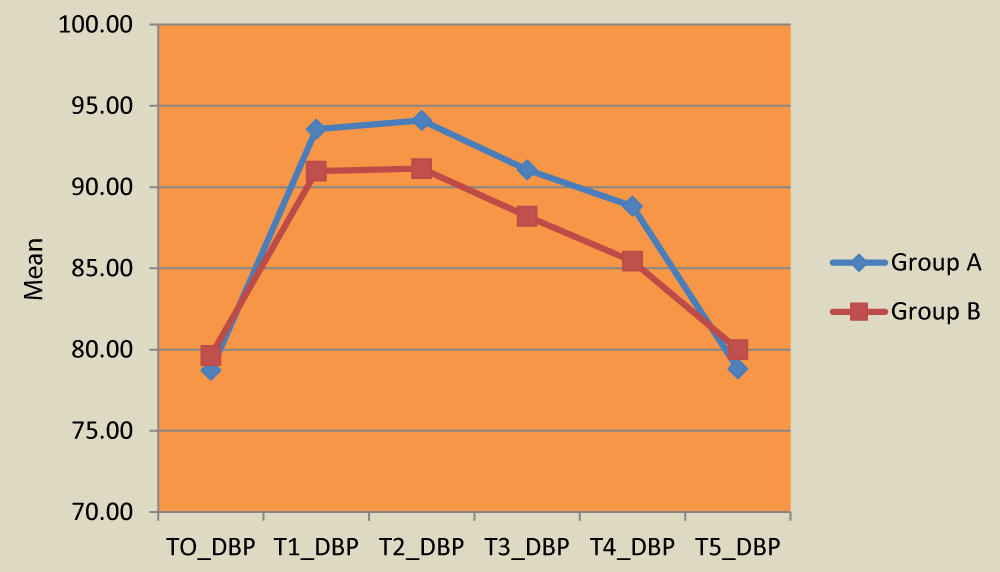
At 2 minutes, 4 minutes and 6 minutes post-intubation, a statistically significant rise in mean heart rate was noted in group A (p = 0.007,0.003,0.008). There was no significant difference with respect to heart rate at 8 minutes and 10 minutes post-intubation. At 2 minutes and 4 minutes difference in mean SBP and DBP of the two groups was statistically significant with a p - value < 0.005 with a significant increase in patients of group A (Table 3). At 6 minutes and 8 minutes post-intubation also, there was a significant change in mean SBP and DBP in group A patients as compared to group B patients (p - value - < 0.005). At 2, 4, 6, and 8 minutes difference in mean MAP of the two groups was statistically significant with a p - value of 0.002, 0.001, 0.000 and 0.000 respectively with a significant change in patients of group A. No significant change in mean SpO2 was observed at different time intervals post-intubation amongst both groups. The difference for all complications such as laryngospasm, bronchospasm, the trauma of lip or tongue, and cough/sore throat was not significant between the two groups (Table 4)(Figures 1-3).
| Table 3: Distribution of hemodynamic parameters at different time intervals in both groups. | |||||
| Group A | Group B | p - value | |||
| Mean | SD | Mean | SD | ||
| HR-TO | 73.54 | 6.88 | 74.94 | 7.70 | 0.340 |
| HR-T1* | 96.52 | 7.60 | 92.36 | 7.63 | 0.007 |
| HR-T2* | 96.96 | 7.40 | 92.56 | 7.17 | 0.003 |
| HR-T3* | 89.82 | 7.61 | 85.72 | 7.51 | 0.008 |
| SBP-TO | 121.84 | 6.41 | 122.64 | 5.52 | 0.505 |
| SBP-T1* | 146.66 | 7.57 | 142.38 | 6.45 | 0.003 |
| SBP-T2* | 146.82 | 7.76 | 142.40 | 6.51 | 0.003 |
| SBP-T3* | 140.96 | 6.62 | 136.70 | 5.59 | 0.001 |
| DBP-TO | 78.72 | 5.15 | 79.64 | 4.88 | 0.362 |
| DBP-T1* | 93.56 | 5.87 | 90.98 | 5.42 | 0.025 |
| DBP-T2* | 94.10 | 5.90 | 91.14 | 5.28 | 0.010 |
| DBP-T3* | 91.06 | 5.73 | 88.20 | 4.87 | 0.008 |
| * p < 0.05 is significant. | |||||
| Table 4: Distribution of complications in both groups. | |||||
| Group a | Group b | p - value | |||
| N | % | N | % | ||
| Laryngospasm | 2 | 4 | 2 | 4 | 1.000 |
| Bronchospasm | 3 | 6 | 2 | 4 | 0.646 |
| Trauma(lip/tongue) | 2 | 4 | 1 | 2 | 0.603 |
| Cough/sore throat | 6 | 12 | 4 | 8 | 0.505 |
Figure 1: Distribution of heart rate at different time periods in both groups.
Figure 2: Distribution of systolic blood pressure at different time periods in both groups.
Figure 3: Distribution of diastolic blood pressure at different time periods in both groups.
It is the duty of an anesthesiologist to ensure a patent airway’s optimum ventilation. Till recently, the cuffed endotracheal tube was considered an ideal method but nowadays many guiding devices have come into action. Endotracheal intubation is done usually by direct laryngoscopy under direct vision, for example with a Macintosh blade. This is conducive to healthy patients but in hypertensive patients or with co-morbidities, it may be hazardous due to an increase in reflex sympathetic activity leading to hypertension and tachycardia. Soon after intubation blood pressure starts rising within 5 seconds and keeps trending upwards to 2 minutes - 5 minutes followed by a return to baseline subsequently. The use of guiding devices leads to the avoidance of distortion of oro-pharyngeal structures or physical stimulus causing a lesser change in hemodynamic parameters.
The study of Bharti N, et al. [10] had concordance in intubation results at the first attempt of 95% and 90% with direct laryngoscopy and ILMA group respectively (p – value = > 0.05). Another such study by Kavitha J, et al. [11] demonstrated that tracheal intubation was successful in the first attempt in 90% of patients in the DLS group versus 83.3% in the ILMA group. Hence, the two groups were comparable with regard to ease of intubation with similar findings in our study.
Similar to our findings, a study by Rastogi B, et al. [12] had mean intubation time in the ILMA group as 85.25 ± 13.19 seconds and 17.25 ± 9.74 seconds in the Macintosh Laryngoscopy group (p – value = < 0.05). A corresponding study by Bharti N, et al. [10] compared the ease of insertion following tracheal intubation through ILMA with that of conventional Macintosh laryngoscope in 80 patients and found that intubation time was comparatively longer in the ILMA group than the laryngoscopy group (59.8 ± 8.7 s versus 35 ± 4.6 s, p < 0.001). These results were of statistical significance.
Differences in intubation time were presumably more due to the lack of expertise of doctors/health care workers performing intubation. Secondly, help given by the assistant is also crucial which aids in two steps that are the insertion of ILMA followed by intubation. Inflation of the ILMA cuff, then deflation of the endotracheal tube cuff for mobility and finally re-inflation after the entrance into the trachea are the steps needed.
In contrast to our study, Sharma MU, et al. [13] performed a study in which the meantime for successful tracheal intubation was 10.04 ± 4.49 seconds via ILMA. This difference from our results is due to the use of wire-reinforced silicone endotracheal tubes.
Our study deciphered that patients in group B showed less hemodynamic response with respect to heart rate to intubation as compared to patients in group A at 2, 4, and 6 minutes post-intubation. Similar to our study findings, a study by Fattah A, et al. [14] in 2015 deduced that there was a higher increase in heart rate for 3 minutes post-intubation as well as post-extubation in a group with Macintosh laryngoscope compared to the ILMA group with significant p - value (< 0.05).
In concordance with our study, Rastogi B, et al. [15] deciphered that heart rate in patients intubated via ILMA increased from baseline till 2 minutes and thereafter showed decreasing trend till 5th-minute post-intubation. A similar significant change in heart rate was observed in the direct laryngoscopy group. The feasible reason attributed to less pressor response in the ILMA group may be that neither epiglottis elevation was required nor Proprio-receptors at the base of the tongue got stimulated.
In contrast to our study, Kihara S, et al. [16] analyzed hemodynamic changes to intubation via ILMA and with a Macintosh laryngoscope in both normotensive and hypertensive patients. There was no statistically significant difference in change in heart rate post-intubation amongst both groups (p > 0.05) in normotensive patients. The reason behind this stipulated was that hypertensive patients have an exaggerated hemodynamic stress response compared with normotensive patients due to increased catecholamine levels, therefore significant heart rate change was not detected clinically in normotensive patients.
In our study, we concluded that usage of intubating laryngeal mask airway is accompanied by minimal cardiovascular responses than those associated with direct laryngoscopic tracheal intubation with Macintosh blade thus making it more helpful in hypertensive patients. Practically, this hemodynamic stress response difference may be there because of the reason that as lesser mechanical force is applied to pharyngeal structures during intubation with ILMA, it must be less stimulating compared to laryngoscope-guided intubation.
In agreement with our study, Siddiqui N, et al. [17] demonstrated hemodynamic response via ILMA or direct laryngoscopy and found that a rise in systolic blood pressure in the direct laryngoscopy group was 26% and 13% when compared with baseline for the first two minutes, while in ILMA group the increase was 8% - 12% (p – value < 0.05). The rise in diastolic blood pressure was 23% and 7% in direct laryngoscopy and ILMA respectively (p < 0.05).
Similar to our study, Gamil S, et al. [18] concluded that the hemodynamics was significantly higher in the DL group versus the ILMA group. The possible reason behind that was serum cortisol and blood glucose levels were significantly higher in the DL group than in the ILMA group. Therefore, ILMA was superior to Macintosh Laryngoscope in attenuation of stress responses to endotracheal intubation so, it is a preferred device for intubation in hypertensive patients according to this study.
Similar to our findings, Wilson IG, et al. [19] also found a significant increase in SBP of 51.3% after tracheal intubation versus 22.9% in the ILMA group. A study done by Aziz L, et al. [20] also collaborated similar findings as our study.
Contradictory to our study findings, in the analysis of changes in SBP and DBP in a study by Jarineshin H, et al. [21], there were no significant changes compared to the baseline at any time interval. A justifiable reason might be that propofol was used for both induction and maintaining anesthesia resulting in greater hypotension compared to sodium thiopental used in other studies.
A study by Sener EB, et al. [22] had higher blood pressure after 4 minutes in the ILMA group which can be attributed to the mechanical stimulus to the supra-laryngeal area, which is rich in nociceptive receptors and can cause strong hemodynamic responses.
The inter-study discrepancies might be due to the use of intravenous lignocaine [23] at the time of induction in few studies or greater depth of anesthesia or various adjusting maneuvers making ILMA insertion a potent sympathetic stimulant or use of another type of endotracheal tubes of softer Fastrack silicone or rigid polyvinyl chloride type. Factors such as force utilized during ILMA insertion, duration, and attempts are also enumerated. ILMA being a lengthy process, it can also lead to excessive capillary perfusion pressure because of compression of pharyngeal structures. Furthermore, this contrasting finding may be due to the loss of stimulatory effects of direct laryngoscopy and intubation, which is usually transient and returns to the control status within 5 minutes after the first insult resulting in no significant difference amongst the groups.
ILMA-guided oro-tracheal intubation has some advantages because this procedure does not distort the base of the tongue or directly stimulate the receptors in the larynx [24]. Theoretically, ILMA-guided oro-tracheal intubation may produce less adverse cardiovascular stress responses.
In agreement with our study, Siddiqui N, et al. [17] demonstrated hemodynamic response via ILMA or direct laryngoscopy and found a statistically significant difference in a rise in mean arterial blood pressure (p < 0.05) after intubation in both groups. Similar to our findings, a study by Tabari M, et al.[25] demonstrated that MAP was significantly higher in patients who were intubated by direct laryngoscopy when compared with ILMA at 5 minutes post-intubation (p = 0.03). They concluded that ILMA may be used for patients in whom a marked pressure response would be undesirable.
Similar results were seen in a study conducted by Fattah A, et al. [26] in which in controlled hypertensive patients MAP increased in both groups with significantly higher and longer-lasting rise after tracheal intubation with laryngoscopy than with ILMA. This may be due to manipulation of the airway altering cardiovascular physiology by means of both reflex response and physical presence of endotracheal tube.
In agreement with our findings, Modir H, et al. [27] studied hemodynamic response in two groups of patients intubated with either ILMA or video-laryngoscopy. They found no statistically significant difference in Sp02 in both groups (p = 0.706).
Similar to our study, Joo HS, et al. [28] found no statistically significant difference in post-operative sore throat and hoarseness via ILMA with or without fiber-optic guidance. In contrast to our study, Dimitriou V, et al. [29] had a higher incidence of mucosal trauma in the ILMA group which may be because of the high pressure exerted by ILMA against pharyngeal mucosa. Furthermore, there was no difference in sore throat or hoarseness incidence in both group.
Intubation via intubating laryngeal mask airway can be done as an alternative to direct laryngoscopy using a Macintosh blade as intubation via intubating laryngeal mask airway has shown to have lesser hemodynamic changes
Limitations
In this study, blind oro-tracheal intubation was done through ILMA. However, in the future fiber-optic guided oro-tracheal intubation through ILMA can also be done, to further attenuate hemodynamic response as well as to have advantages like a lesser number of attempts and less time of insertion. Also, we have not taken into account anticipated difficult airways in our study. Results might vary if a difficult airway may also be included in the inclusion criteria.
- Buhari FS, Selvaraj V. Randomized controlled study comparing the hemodynamic response to laryngoscopy and endotracheal intubation with McCoy, Macintosh, and C-MAC laryngoscopes in adult patients. J Anaesthesiol Clin Pharmacol. 2016 Oct-Dec;32(4):505-509. doi: 10.4103/0970-9185.194766. PMID: 28096584; PMCID: PMC5187618.
- Brain AI, Verghese C, Addy EV, Kapila A. The intubating laryngeal mask. I: Development of a new device for intubation of the trachea. Br J Anaesth. 1997 Dec;79(6):699-703. doi: 10.1093/bja/79.6.699. PMID: 9496198.
- Altun D, Ali A, Çamcı E, Özonur A, Seyhan TÖ. Haemodynamic Response to Four Different Laryngoscopes. Turk J Anaesthesiol Reanim. 2018 Dec;46(6):434-440. doi: 10.5152/TJAR.2018.59265. Epub 2018 Sep 6. PMID: 30505605; PMCID: PMC6223868.
- Kihara S, Watanabe S, Taguchi N, Suga A, Brimacombe JR. A comparison of blind and lightwand-guided tracheal intubation through the intubating laryngeal mask. Anaesthesia. 2000 May;55(5):427-31. doi: 10.1046/j.1365-2044.2000.01324.x. PMID: 10792132.
- Stone DJ, Gal TJ. Airway Management. In Miller RD ed. Anesthesia. 5th ed. Churchill Livingstone New York. 2000; 39:1444-5.
- Kovac AL. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1996 Feb;8(1):63-79. doi: 10.1016/0952-8180(95)00147-6. PMID: 8695083.
- Pollard BJ, Norton ML. Principles of Airway Management, In: Wylie and Churchill – Davidson’s, A Practice of Anesthesia (7th Edn) 2003; 28: 445-6.
- Rosenblatt WH. Airway Management. In: Barash PG, Cullen BF, Stoelting RK. Clinical Anesthesia (4th Edn). 2001; 23: 599-605.
- Kahl M, Eberhart LH, Behnke H, Sänger S, Schwarz U, Vogt S, Moosdorf R, Wulf H, Geldner G. Stress response to tracheal intubation in patients undergoing coronary artery surgery: direct laryngoscopy versus an intubating laryngeal mask airway. J Cardiothorac Vasc Anesth. 2004 Jun;18(3):275-80. doi: 10.1053/j.jvca.2004.03.005. PMID: 15232805.
- Bharti N. Clinical investigation ease of insertion and haemodynamic effects following tracheal intubation using intubating laryngeal mask airway: a comparison with conventional macintosh laryngoscope Indian J. Anaesth. 2006; 50: 205-8.
- Kavitha J, Tripathy DK, Mishra SK, Mishra G, Chandrasekhar LJ, Ezhilarasu P. Intubating condition, hemodynamic parameters and upper airway morbidity: A comparison of intubating laryngeal mask airway with standard direct laryngoscopy. Anesth Essays Res. 2011 Jan-Jun;5(1):48-56. doi: 10.4103/0259-1162.84190. PMID: 25885300; PMCID: PMC4173360.
- Rastogi B, Singh VP, Gandhi A, Jain M, Gupta K, Singh M, et al. Comparative evaluation of hemodynamic response with intubating laryngeal mask airway and intubation with Macintosh Blade- A prospective study. Glob Anaesth Perioper Med. 2015; 1: 34-9.
- Sharma MU, Gombar S, Gombar KK, Singh B, Bhatia N. Endotracheal intubation through the intubating laryngeal mask airway (LMA-Fastrach™): A randomized study of LMA- Fastrach™ wire-reinforced silicone endotracheal tube versus conventional polyvinyl chloride tracheal tube. Indian J Anaesth. 2013 Jan;57(1):19-24. doi: 10.4103/0019-5049.108555. PMID: 23716761; PMCID: PMC3658329.
- Abdel Fattah MM. Comparison of hemodynamic response to tracheal intubation with laryngoscope versus intubating laryngeal mask airway in elderly hypertensive patients. Ain-Shams J Anaesthesiol. 2016; 9:34-8.
- Rastogi B, Singh VP, Gandhi A, Jain M, Gupta K, Singh M, et al. Comparative evaluation of hemodynamic response with intubating laryngeal mask airway and intubation with Macintosh Blade- A prospective study. Glob Anaesth Perioper Med. 2015; 1: 34-9.
- Kihara S, Brimacombe J, Yaguchi Y, Watanabe S, Taguchi N, Komatsuzaki T. Hemodynamic responses among three tracheal intubation devices in normotensive and hypertensive patients. Anesth Analg. 2003 Mar;96(3):890-895. doi: 10.1213/01.ANE.0000048706.15720.C9. PMID: 12598280.
- Siddiqui NT, Khan FH. Haemodynamic response to tracheal intubation via intubating laryngeal mask airway versus direct laryngoscopic tracheal intubation. J Pak Med Assoc. 2007 Jan;57(1):11-4. PMID: 17319412.
- Gamil S, Gafaar T, Farid D, Amin O. Intubation Characteristics and Stress Responses during Endotracheal Intubation by Intubating Laryngeal Mask Airway versus Macintosh Laryngoscope in Controlled Hypertensive Patients. Zagazig University Medical Journal. 2019; 14: 45-9.
- Wilson IG, Fell D, Robinson SL, Smith G. Cardiovascular response to insertion of the laryngeal mask. Anesthesia. 1992; 47:200–2.
- Aziz L, Bashir K. Comparison of armoured laryngeal mask airway with endotracheal tube for adenotonsillectomy. J Coll Physicians Surg Pak. 2006 Nov;16(11):685-8. PMID: 17052415.
- Jarineshin H, Kashani S, Vatankhah M, Abdulahzade Baghaee A, Sattari S, Fekrat F. Better Hemodynamic Profile of Laryngeal Mask Airway Insertion Compared to Laryngoscopy and Tracheal Intubation. Iran Red Crescent Med J. 2015 Aug 12;17(8):e28615. doi: 10.5812/ircmj.28615. PMID: 26430529; PMCID: PMC4587401.
- Sener EB, Ustun E, Ustun B, Sarihasan B. Hemodynamic responses and upper airway morbidity following tracheal intubation in patients with hypertension: conventional laryngoscopy versus an intubating laryngeal mask airway. Clinics (Sao Paulo). 2012;67(1):49-54. doi: 10.6061/clinics/2012(01)08. PMID: 22249480; PMCID: PMC3248601.
- Hamaya Y, Dohi S. Differences in cardiovascular response to airway stimulation at different sites and blockade of the responses by lidocaine. Anesthesiology. 2000 Jul;93(1):95-103. doi: 10.1097/00000542-200007000-00018. PMID: 10861151.
- Wong JK, Tongier WK, Armbruster SC, White PF. Use of the intubating laryngeal mask airway to facilitate awake orotracheal intubation in patients with cervical spine disorders. J Clin Anesth. 1999 Jun;11(4):346-8. doi: 10.1016/s0952-8180(99)00052-5. PMID: 10470641.
- Masoomeh T, Mohammed A, Almadi M. Hemodynamic changes occurring with tracheal intubation by direct laryngoscopy compared with intubating laryngeal mask airway in adults: a random comparison trial. Egypt J Anesthesia. 2013; 29:103-7.
- Abdel Fattah MM. Comparison of hemodynamic response to tracheal intubation with laryngoscope versus intubating laryngeal mask airway in elderly hypertensive patients. Ain-Shams J Anaesthesiol. 2016; 9:34-8.
- Modir H, Moshiri E, Malekianzadeh B, Noori G, Mohammadbeigi A. Endotracheal intubation in patients with difficult airway: using laryngeal mask airway with bougie versus video laryngoscopy. Med Gas Res. 2017 Oct 17;7(3):150-155. doi: 10.4103/2045-9912.215744. PMID: 29152207; PMCID: PMC5674652.
- Joo HS, Kapoor S, Rose DK, Naik VN. The intubating laryngeal mask airway after induction of general anesthesia versus awake fiberoptic intubation in patients with difficult airways. Anesth Analg. 2001 May;92(5):1342-6. doi: 10.1097/00000539-200105000-00050. PMID: 11323374.
- Dimitriou V, Voyagis GS, Brimacombe JR. Flexible lightwand-guided tracheal intubation with the intubating laryngeal mask Fastrach in adults after unpredicted failed laryngoscope-guided tracheal intubation. Anesthesiology. 2002 Feb;96(2):296-9. doi: 10.1097/00000542-200202000-00012. PMID: 11818759.