More Information
Submitted: September 14, 2022| Approved: September 19, 2022 | Published: September 20, 2022
How to cite this article: Yasmina NP, Lisseth HGV, Marcio BSA. A case report of hepatic actinomycosis: A rare form of presentation. Int J Clin Anesth Res. 2022; 6: 004-006.
DOI: 10.29328/journal.ijcar.1001019
Copyright License: © 2022 Yasmina NP, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Liver abscesses; Hepatic actinomycosis; Acute abdominal pain; Penicillin
Abbreviations: HA: Hepatic Actinomycosis
A case report of hepatic actinomycosis: A rare form of presentation
Nieto Piñar Yasmina1, Hernández González Verónica Lisseth1 and Borges SA Marcio2*
1Multidisciplinary Sepsis Unit, Intensive Care Unit, Son Llàtzer University Hospital, Spain
2Associate Professor of Infectious Diseases, Multidisciplinary Sepsis Unit, Intensive Care Unit, Son Llàtzer University Hospital, Spain
*Address for Correspondence: Borges SA Marcio, Associate Professor of Infectious Diseases, Multidisciplinary Sepsis Unit, Intensive Care Unit, Son Llàtzer University Hospital, Spain, Email: [email protected]; [email protected]
Hepatic Actinomycosis (HA) is a very rare abdominal actinomycosis that can be confused with hepatic involvement due to a tumor. Liver involvement can occur from an abdominal focus or by blood dissemination from another focus. This disease is much more common in men between 50 - 70 years and in a situation of immunosuppression.
Symptoms are nonspecific and diagnosis includes histopathology, cultures, and imaging test. Treatment includes prolonged antibiotic therapy with antibiotics such as penicillin and drainage of abscesses.
We present a case of a 54-year-old man patient with a record of three years of chronic pancreatitis of probably alcoholic origin, who developed hepatic actinomycosis, requiring drainage of liver abscesses and directed antibiotic treatment.
Actinomyces spp. is opportunistic gram-positive, anaerobic, or facultatively anaerobic bacteria that usually colonize the upper respiratory tract or the gastrointestinal and female genital tract and typically infect males between 50 and 70 years old [1]. The diagnosis of suspicion is complicated because the history and clinical presentation are not specific for this rare entity [1-3]. Evolution is slow and steady in inflammatory contiguous extension without limitation on one organ, character prone to confusion with abdominal malignancies [2,4].
A 54-year-old man presented at the emergency department with a history of abdominal pain, fever, and nausea two-day evolution.
His personal history includes sacral fistulae, chronic pancreatitis of probable alcoholic origin complicated with pancreatic cystic lesions, cholelithiasis and exocrine pancreatic insufficiency.
On his physical examination, he had a blood pressure of 60/40 mmHg, a heart rate of 95bpm, and abdominal pain localized in the right hypochondrium. Empirical antibiotic therapy with ertapenem and fluid therapy was started.
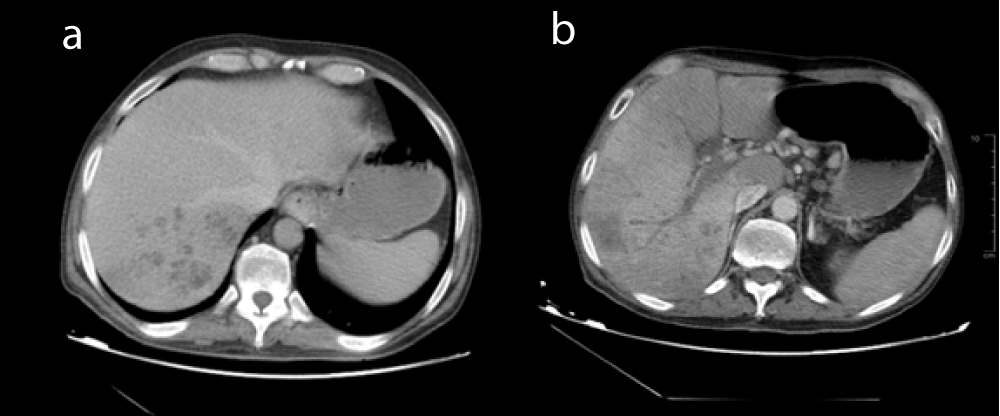
The abdominal CT scan (Figure 1) described extensive portal vein thrombosis with carcinomatosis and congestive liver with numerous hypodense lesions in the right lobe that may correspond to poorly defined microabscesses. Images compatible with chronic pancreatitis and dilatation of the bile duct.
Figure 1: Abdominal CT (a): Hepatic Abscess: congestive liver with numerous hypodense lesions in the right lobe that may correspond to poorly defined microabscesses. (b): Extensive portal vein thrombosis with carcinomatosis.
Blood analysis revealed: Leukocytosis 20, 60 10^9/L [normal 4.00-11.00] with neutrophilia. Hb 9.11 gr/dl [normal 13,00 - 16.7] Coagulopathy INR 1.79 [normal 0.7-1.20], PT 45% [normal 70-120], acute renal failure with creatinine 2.03 mg/dl [normal 0.7-1.25] and Urea 77 mg/dl [normal 18-55], GFR 36 ml/min, hyperlactacidemia 5.43 mmol/l [normal 0.5-2.2]. Total Bilirubin 1.85 mg/dl normal [0.2-1.2], Direct Bilirubin 1.27 mg/dl [normal 0.0-0.5], AST 1494 U/L [normal 5-34], ALT 389 U/l[normal 1-55], C-Reactive Protein 178.90 mg/l [normal 0.0-5], Procalcitonin 189.46 ng/ml [0.0-0.05].
The patient is oriented as a septic shock of biliary and hepatic origin, and he is admitted to the Intensive Care Unit. Blood cultures were taken and hemodynamic support was started (requiring high doses of vasoactive drugs), corticosteroids, empirical antibiotic therapy with piperacillin/tazobactam and linezolid and anticoagulation with low heparin molecular weight.
The endoscopic retrograde cholangiopancreatography revealed chronic pancreatitis with associated choledochal stenosis. Cystic dystrophy of the duodenal wall (groove pancreatitis) for which a plastic biliary prosthesis was placed.
After five days, abdominal CT was repeated: formation of a well-defined collection, probable abscess in hepatic segment VI with a 4.5 cm long axis; numerous small lesions (up to 1.5 cm) in segments VI and VII, hepatic portal thrombosis persists, patent splenic vein, biliary prosthesis, no notable dilatation of the bile duct is observed.
After these results, it was decided to place two Pigtail drainage catheters into the two largest hepatic collections obtaining seropurulent fluid.
In blood, cultures grow Actinomyces turicensis, Eikenella corrodens, and Gemella morbillorum. In hepatic abscess, culture grows Actinomyces turicensis, Eikenella corrodens.
Finally, a control CT scan was performed a month later, watching the disappearance of most of the hepatic collections with just one persisting in segment VI of smaller size. The patient received antibiotic treatment for four weeks with amoxicillin-clavulanate first intravenously and later with oral amoxicillin. The patient was discharged one month later without antibiotic therapy. The biliary prosthesis was removed two months later.
The patient continues with the follow-up after five years after the infection.
HA is a very rare abdominal actinomycosis and generally occurs after an abdominal infection. The infection is much more common in men between 50 and 70 years as the most susceptible group [1,3].
While any site in the body can be involved with actinomycosis, cervicofacial infection is the most common one. Other parts of the body prone to be infected with Actinomyces spp. are the thorax, abdomen, pelvis, and central nervous system. Abdominal infection occurs in 20% of cases and the appendix and the ileocecal region are generally affected [2,5,6]. Hepatic involvement is usually uncommon and occurs in only 5% of all actinomycosis cases [1]. Liver involvement may occur from an extension of contiguous abdominal focus or by hematogenous spread via the portal vein [7]. In other cases, the infection may be due to mucosal injury induced by surgical or endoscopic manipulation, ulcer, foreign bodies, or immunosuppression [3,4]. In our case, the route of dissemination probably occurs associated with cholangitis. However, complications such as portal vein thrombosis have been described [3] as they could be in our patients.
In addition, the coexistence of this infection with other microorganisms is frequent (Streptococcus, Peptostreptococcus, Staphylococcus, Neisseria, and Aspergillus among others), which might be explained by immunological inhibition of the host [1,5]. In our case, in blood cultures grow Actinomyces turicensis, Eikenella corrodens, and Gemella morbillorum. In hepatic abscess, culture grows Actinomyces turicensis, Eikenella corrodens.
Diagnosis of HA is often challenging because infection diagnosis is dependent on clinical manifestations and findings from imaging. Symptoms of HA are nonspecific and variable and include abdominal pain, fever, and anorexia [1,3]. Imaging tests are also unspecific and often mimic a primary or metastatic tumor on the liver [1,2]. Particularly in ultrasound, CT and MRI, hepatic actinomycosis presents with a single hypodense lesion in 66% of cases. In the remaining 33%, it may present as multiple hepatic abscesses [7]. In about 44.7% of the cases mimics a malignant lesion and the right lobe is the most affected (56.5%) [7]. Nevertheless, in our case, the CT describes defined extensive portal vein thrombosis with carcinomatosis and congestive liver with numerous hypodense lesions in the right lobe that may correspond to poorly defined microabscesses.
The final diagnosis is made on pathophysiology, demonstrating the presence of aggregates of filamentous Gram-positive in sulfur granules [1,3]. In a small percentage, they can be identified in cultures this is due either to previous antimicrobial treatment or adequate culture conditions [2]. MALDI-TOF and PCR can also be used for direct detection [1,5]. In our case, the diagnosis was obtained by cultures of the liver abscess drainage.
Therapeutic management includes antibiotics, drainage of the abscess, and resection if it is necessary. Long antimicrobial treatment is recommended to avoid recurrence [1,3,6]. Penicillin is the indicated treatment and must be given intravenously during 4-6 weeks, followed by oral penicillin for months. [1,3,4,7]. Other drugs can be doxycycline, cephalosporins, and tetracyclines [3,6]. In our case, treatment included percutaneous drainage and intravenous therapy, followed by oral therapy for one month.
Finally, the duration of treatment should be individualized based on disease location, severity, and changes in follow-up imaging [1,3,7].
We present a case of this rare disease with very few cases published in the literature.
HA is a difficult disease to diagnose due to. In many patients, this infection is confused with other diseases, which may lead to extensive surgery, so abdominal actinomycosis should always be included in the differential diagnosis of abdominal tumors.
The treatment of choice is penicillin, the duration ranges from weeks to months, with a trend toward shorter therapeutic cycles; however, the existing evidence of the duration of treatment is limited.
- Chegini Z, Didehdar M, Tabaeian SP, Khoshbayan A, Shariati A. A systematic review of case reports of hepatic actinomycosis. Orphanet J Rare Dis. 2021 Apr 30;16(1):192. doi: 10.1186/s13023-021-01821-5. PMID: 33931097; PMCID: PMC8086304.
- Târcoveanu E, Vasilescu A, Andronic D, Lupaşcu C, Ciobanu D, Vlad N, Bradea C. Abdominal Actinomycosis Mimicking Colon Cancer. Chirurgia (Bucur). 2019 Mar-Apr;114(2):251-258. doi: 10.21614/chirurgia.114.2.251. PMID: 31060658.
- Maraki S, Mavromanolaki VE, Stafylaki D, Anagnostopoulou E, Moraitis P, Kasimati A, Treptow B. A 60-Year Literature Review on Hepatic Actinomycosis. Med Princ Pract. 2022;31(2):103-110. doi: 10.1159/000521990. Epub 2022 Jan 17. PMID: 35038716; PMCID: PMC9209987.
- Albayrak A, Ozkurt Z, Ozden K. Hepatic actinomycosis: a very rare form of actinomycosis. Rev Soc Bras Med Trop. 2021 Mar 8;54:e0289-2020. doi: 10.1590/0037-8682-0289-2020. PMID: 33681913; PMCID: PMC8008916.
- Manterola C, Grandes L, Riffo-Campos AL, Salgado C, Otzen T. Clinical aspects of abdominal actinomicosis: a systematic review. ANZ Journal of Surgery. 2020; 90(7-8):1465-1468.
- Tarzi M, Douedari A, Aldakhil R, Danial AK, Al-Haj A. Case report: actinomicosis of the abdominal wall. Journal of Surgical Case Reports. 2021; 5:1-3.
- Ávila F, Santos V, Massinha P, Pereira JR, Quintanilha R, Figueiredo A, Lázaro A, Carrelho S, Coelho JS, Barroso E, Duarte MA. Hepatic Actinomycosis. GE Port J Gastroenterol. 2015 Jan 7;22(1):19-23. doi: 10.1016/j.jpge.2014.08.002. PMID: 28868364; PMCID: PMC5580170.