More Information
Submitted: 26 August 2020| Approved: 28 September 2020 | Published: 29 September 2020
How to cite this article: Asci SS, Eroglu A, Asci C. A comparison of complications associated with nutrition between the patients receiving enteral or parenteral in the intensive care unit. Int J Clin Anesth Res. 2020; 4: 013-018.
DOI: 10.29328/journal.ijcar.1001015
ORCiD: orcid.org/0000-0002-0396-1582
Copyright License: © 2020 Asci SS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Enteral nutrition; Parenteral nutrition; Complication; Mortality; Morbidity; ICU
A comparison of complications associated with nutrition between the patients receiving enteral or parenteral in the intensive care unit
Seyhan Sumeyra Asci, Ahmet Eroglu* and Coskun Asci
Karadeniz Technical University, Anesthesiology and Intensive Care Medicine, Trabzon, Turkey
*Address for Correspondence: Dr. Ahmet Eroglu, Karadeniz Technical University, Anesthesiology and Intensive Care Medicine, Trabzon, Turkey, Email: [email protected]
The aim of this study was to investigate and compare the complications including infection and mortality associated with enteral and parenteral nutrition on patients in the ICU of a university hospital.
In this study, a total of 100 patients who were under follow-up in the ICU for two years were examined. In our study, demographic characteristics, the reason for admission, comorbidity, initial ICU laboratory values, morbidity and mortality during the follow-up period of the patients who only received enteral nutrition (EN) or parenteral nutrition (PN) were evaluated, and the results between two were compared as well as evaluating the complications within the groups.
The comparison of the reason for admission between the EN and PN groups showed that surgical reasons were significantly higher in the PN group. Nosocomial infections, the presence of infection and the development of sepsis were significantly higher in the EN group. The 28-day mortality rate was higher in the PN group compared to the EN group. The length of stay in the ICU and on mechanical ventilation was longer in the EN group. There was no significant difference in the 28-day mortality, readmission to the ICU and repeated endotracheal intubation between the two groups.
Because there is no statistical difference between EN and PN groups in point of infection and mortality, we conclude that the length of stay in the ICU and reason for admission play a more crucial role in the development of infection and on mortality rather than enteral or parenteral nutrition route.
Nutrition support is one of the most important parameters in the Intensive Care Unit (ICU). Nutrition support is known to affect mortality and morbidity; help wound healing and have positive effects on the immune system. While it serves only as a supportive treatment for elective patients, it can increase the survival rate of critically ill patients, when applied correctly and at right time. Oral feeding is the normal route of nutrition; however, it is often not possible in ICU patients. Enteral and parenteral nutrition were developed for such cases [1,2].
In recent years, researchers have been emphasizing the importance of early enteral nutrition for intensive care unit patients. Enteral nutrition (EN) is usually recommended and preferred as it protects the structure and functions of the gastrointestinal tract, is the physiological route, has fewer complications and lower costs [3-6].
The role of nutrition support in patient care has become an important factor in medicine as the studies conducted over the last 50 years revealed its benefits, such as prevention of many complications. There are a number of studies comparing enteral (EN) and parental nutrition (PN) and they showed that parenteral nutrition caused more complications in intensive care patients compared to enteral nutrition [7].
In our study, we aimed to reveal the complications in patients who were only fed enterally or parenterally, and to compare the length of stay in hospital and ICU, length of stay on mechanical ventilation, the incidence rate of infection and mortality and morbidity in patients who only received enteral or parenteral nutrition.
After the approval of the local ethics committee of a university was obtained, the patients who were under follow-up and treatment in the Anesthesiology Intensive Care Unit for two years were retrospectively analyzed. Authors’ institutional review board (IRB) has approved the study.
In this study, a total of 100 patients who were under follow-up or treatment in Anesthesiology Intensive Care Unit (ICU) of a university hospital for two years were examined. In our study, demographic characteristics, the reason for admission, comorbidity, initial ICU laboratory values, morbidity during the follow-up period of the patients who received enteral nutrition (EN) or parenteral nutrition (PN) were evaluated as well as examining the complications which are related to the groups.
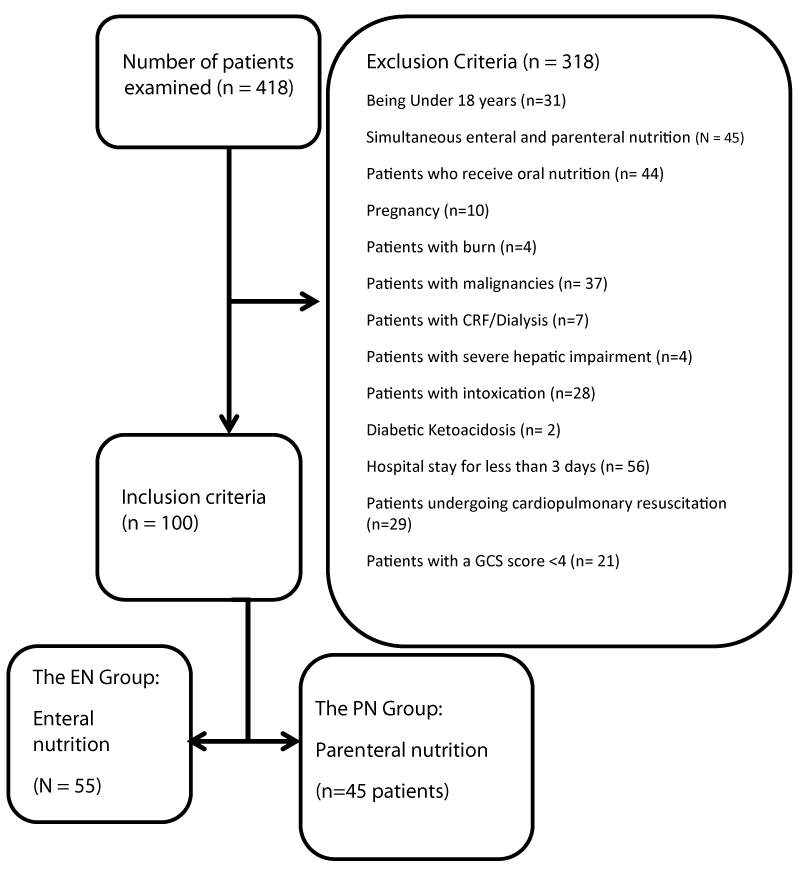
The exclusion criteria were as follows: being under 18 years, receiving both enteral and parenteral nutrition simultaneously, oral feeding, pregnancy, and suffering from burn, malignancy, chronic renal failure (CRF), severe hepatic insufficiency, intoxication, diabetic ketoacidosis, the patient with cardiopulmonary resuscitation, Glasgow coma score (GCS) < 4 and the patients who stayed less than three days in hospital.
EN group included patients who only had enteral nutrition during the whole period in the intensive care unit, while PN Group included patients who only had parenteral nutrition because of surgical causes. A total of 100 patients who met inclusion criteria were included in the study. EN group included 55 patients and PN group included 45 patients in CONSORT Diagram (Diagram 1).
Diagram 1: CONSORT Diagram.
The demographics characteristics [age, gender, Body Mass Index (BMI)], reason for admission [medical causes (cardiac, neurological, respiratory, sepsis, gastrointestinal system) and surgical causes (trauma and postoperative)], comorbid diseases [gastrointestinal system (GIS), hypertension (HT), coronary artery disease (CAD), congestive heart failure (CHF), diabetes mellitus (DM), renal, chronic obstructive pulmonary disease (COPD), neurological and hematological], admission laboratory values [creatinine, platelet, INR (international normalized ratio), bilirubin, oxygenation status (PO2/ FiO2), glucose], APACHE II scores (Acute Physiology and Chronic Health Evaluation II) and GCS were recorded. The following comorbidities were noted during the follow-up period: nosocomial infections (NI), anemia (hemoglobin < 7 g/dL), erythrocyte suspension (ES) requirement, suffer from disseminated intravascular coagulation (DIC) (INR > 1.5, platelet < 100000), renal replacement therapy requirement (RRT), hyperbilirubinemia, vasopressor requirement, steroid therapy related with septic shock, presence of infection, sepsis development, septic shock, septic shock recovery, 28-day mortality, readmission to intensive care unit (ICU), and repeated endotracheal intubation (EI). The length of septic shock, mechanical ventilation and intensive care unit stay were recorded per day.
The complications associated with enteral nutrition (EN) were determined as mechanical, metabolic and gastrointestinal complications.
The complications associated with parenteral nutrition (PN) were determined as catheter-related, metabolic and gastrointestinal complications. The bilirubin levels in the sequential organ failure assessment (SOFA) score were used to evaluate the hepatic disfunction for the gastrointestinal complications. Metabolic complications included hyperglycemia (blood glucose > 180 mg/dL), hypoglycemia (blood glucose < 70 mg/dL), hypernatremia (serum sodium > 145 mEq/L) and hypophosphatemia (serum phosphate < 2.5 mg/dL).
Statistical analysis
Statistics package program was used for statistical analyses of the data obtained in the study. Pearson’s Chi-square test and Fisher’s exact test were used to compare the categorical data. The t-test was used for the comparison of the groups.
The results were evaluated in a 95% confidence interval and p < 0.05 was accepted as statistically significant.
There was no statistically significant difference in gender (p = 0.270 > 0.05), BMI (p = 0.488 > 0.05), age and mean GCS (p > 0.05) between the groups. There was no statistically significant difference in initial APACHE II score, the levels of creatinine, platelets, bilirubin, PaO2/FiO2 and blood glucose levels at admission (p > 0,05) (Table 1).
| Table 1: Data of the Groups at admission. | |||
| Group EN (n = 55) | Group PN (n = 45) | p value | |
| Age (year) | 57.4 ± 22.0 | 56.1 ± 21.0 | 0.76 |
| Gender (M/F) | 28/17 | 24/21 | 0.27 |
| BMI (kg/m2) | 22 | 24 | 0.48 |
| APACHE II | 14.15 ± 5.6 | 15.67 ± 5.9 | 0.18 |
| GKS (3-15) | 11.1 ± 2.5 | 11.2 ± 2.6 | 0.41 |
| PaO2/FiO2 | 297.8 ± 116 | 268.2 ± 107.9 | 0.19 |
| Creatinine | 1.16 ± 0.8 | 1.02 ± 0.6 | 0.33 |
| Glucose | 164.8 ± 65.6 | 158.5 ± 49.2 | 0.59 |
| Platelet | 236945 ± 105072 | 224888 ± 134765 | 0.34 |
| INR | 1.81 ± 1.5 | 1.57 ± 0.54 | 0.27 |
| Bilirubin | 0.89 ± 0.7 | 1.25 ± 1.1 | 0.13 |
There was a statistical difference in reason for admission between the EN and PN groups (p = 0.001). Of the patients in EN group, 35 (63.6%) were admitted to hospital for surgical and 20 (36.4%) patients were admitted for medical causes while of the patients in the PN group, 41 (91.1%) were admitted to hospital for surgical and 4 (8.9%) patients were admitted for medical causes. Surgical admission rate was higher in the PN group while medical admission rate was higher in the EN group.
The rate of admission due to cardiac diseases (p = 0.013) and neurological (p = 0.010) diseases were higher in the EN group.
Postoperative admission was statistically higher in the PN group (p < 0.001).
There was no significant difference in comorbid diseases between the groups. However, if the comorbidities were to be categorized into subgroups; no significant difference was found in HT, CAD, CHF, DM, renal, COPD, neurological diseases between the EN and PN groups similarly (p > 0.05). However, GIS (p = 0.014) and hematologic (p = 0.038) diseases were significantly higher in the PN group than the EN group.
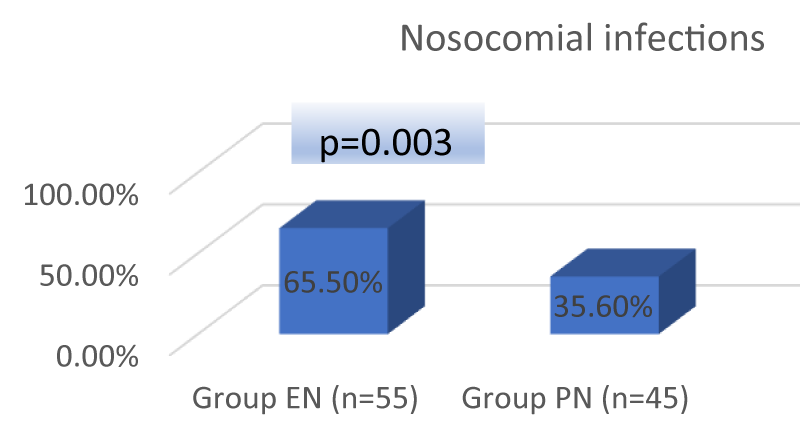
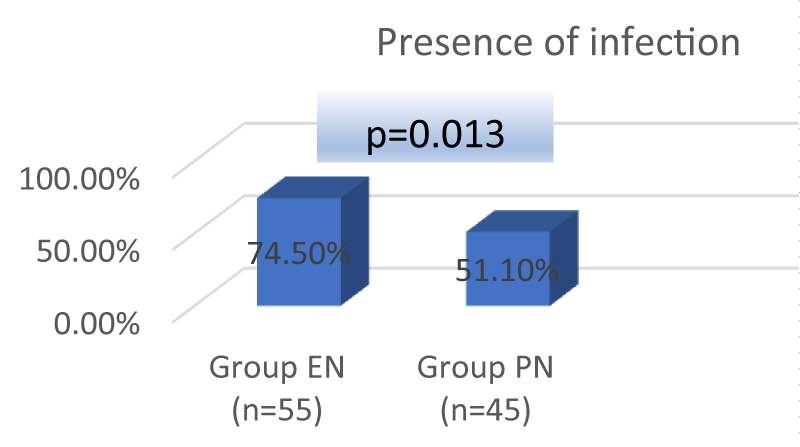
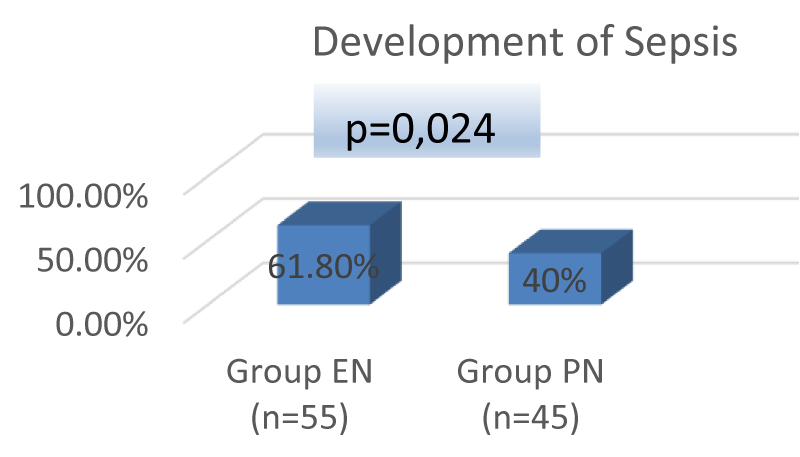
NI development (p = 0.003), presence of infection (p = 0.013) and development of sepsis (p = 0.024) were significantly higher in EN group (Figures 1-3).
Figure 1: Evaluation of the Groups Based on Nosocomial Infections.
Figure 2: Evaluation of the Groups Based on the Presence of Infection.
Figure 3: Evaluation of the Groups Based on Sepsis.
There was no significant difference between the groups in terms of anemia, ES requirement, the occurrence of DIC, renal replacement therapy, hyperbilirubinemia, vasopressor requirement, steroid therapy, septic shock, septic shock recovery, 28-day mortality, readmission to the ICU and repeated ET (p > 0.05).
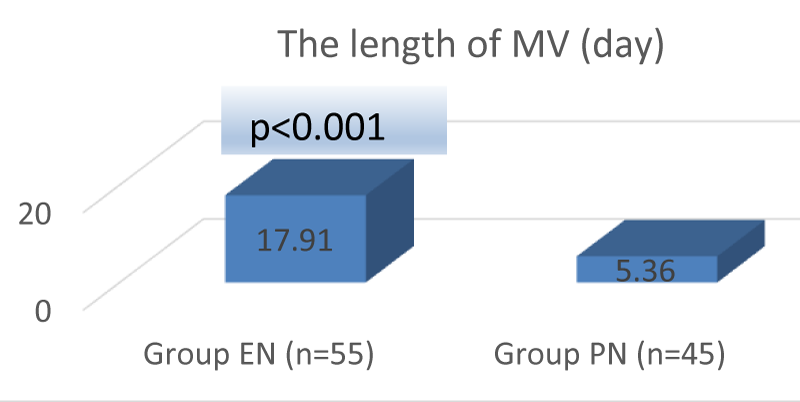
The length of stay on MV was significantly longer in the EN group (17.91 days) than the PN group (5.36 days) (t = 3.703; p < 0.001), (Figure 4).
Figure 4: Evaluation of the Groups Based on Length of Stay (Day) on Mechanical Ventilation.
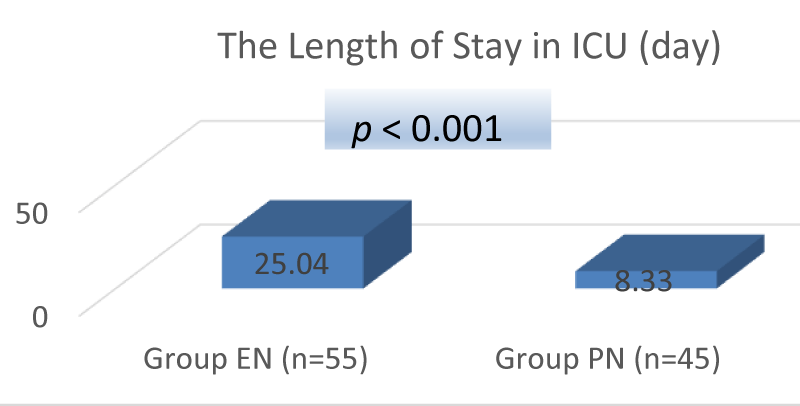
Length of stay in ICU was significantly longer in the EN group (25.04 days) than the PN group (8,33 days) (t = 3.719; p < 0.001), (Figure 5).
Figure 5: Evaluation of the Groups Based on Length of Stay (Day) in ICU.
The comparison of duration of septic shock revealed no significant differences between the groups (p > 0.05).
There was no significant difference in hypoglycemia, hyperglycemia, electrolyte imbalance (hypernatremia, hypophosphatemia) between two groups (p > 0.05).
Of 55 patients in EN group, 48 (87.3%) had nasogastric feeding tube and 7 (12.7%) had percutaneous feeding tube [(percutaneous endoscopic gastrostomy (PEG)/ percutaneous endoscopic jejunostomy (PEJ)].
In the EN group, 12 (21.8%) patients developed mechanical complications; 5 (9.1%) patients developed aspiration pneumonia and 10 (18.2%) patients developed tube obstruction.
In the EN group, 27 patients (49.1%) developed nausea, 18 (32.7%) had vomiting, 20 (36.4%) had diarrhea and 37 (67.3%) had constipation (Table 2).
| Table 2: The complications and 28-day mortality of the EN and PN groups. | |||
| Group EN (n = 55) | Group PN (n = 45) | p value | |
| Mechanical complications (patient) | 12 | 6 | p < 0.05 |
| Tube obstruction (number) | 10 | - | |
| Aspiration pneumonia (number) | 5 | - | |
| Pneumothorax (number) | - | 1 | |
| Arterial puncture (number) | - | 1 | |
| Abscess/hematoma (number) | - | 2 | |
| Obstructions of a central venous catheter (number) | - | 2 | |
| Nausea (number) | 27 | - | |
| Vomiting (number) | 18 | - | |
| Diarrhea (number) | 20 | - | |
| Constipation (number) | 37 | - | |
| 28-day mortality | 23.6% | 28.9% | p = 0.356 |
Of 45 patients in the PN group, 6 (13.3%) developed mechanical complications (1 pneumothorax, 1 arterial puncture, 2 abscess/hematoma, 2 obstructions of a central venous catheter). In addition, 3 (6.7%) patients had catheter-associated sepsis and 13 (28.9%) developed hepatic dysfunction (Table 2).
The difference between the mean APACHE II scores (18.23 ± 5.46) of the patients with 28-day mortality (n = 26) and the mean APACHE II scores (14.83 ± 5.79) of the total of 100 patients was significantly higher in patients with 28-day mortality (p = 0.008).
The comparison of 28-day mortality revealed no statistically significant difference between the groups; however, they were slightly higher in the PN group versus EN group (28.9% vs. 23.6%, p = 0.356) (Table 2).
Enteral nutrition (EN) should be preferred for patients with functional GI disorders [8]. Parenteral nutrition (PN) is an important method for nourishing patients who suffer gastrointestinal tract disorders of diseases or who are unable to be fed by enteral route. It is proved that the proper use of PN has positive effects on the clinical course; however, improper use may lead to increase in infectious complications, development of metabolic anomalies and increased medical costs [9]. In Liu, et al. study [10] on 60 patients with pancreatic cancer, the postoperative group only received enteral nutrition, while the other group received parenteral nutrition. Age, gender and BMI from demographic characteristics revealed no significant difference. Our study showed no significant difference in demographic characteristics.
In their randomized study conducted on 2388 patients, Harvey, et al. [11] compared the correlation of early nutrition with the EN and PN groups and reported that there was no significant difference in the APACHE II scores of the patients at admission. In our study, there was also no significant difference between the APACHE II scores at admission of 100 patients.
Grau, et al. [12] conducted a retrospective cohort study on 725 patients with hepatic dysfunction; they compared two groups who receive EN and PN. It was detected that the reason for admission in the EN group was mostly medical treatment, while surgical admissions were higher in the PN group. Similarly, the comparison of the reason for ICU admission revealed that surgical admissions were significantly higher in the PN group than the EN group in our study.
A retrospective study carried out by Tao, et al. [13] revealed that there was no significant difference between early EN and PN in terms of comorbid diseases (HT, CAD, DM, steatosis hepatitis, COPD, etc.). In our study, only comorbid diseases with higher incidence rates were GI and haematological diseases in the PN group and similarly there are no difference between the groups for HT, CAD, DM, COPD.
In the study was conducted by Harvey, et al. [11], they reported no statistical difference in infectious complications between the EN and PN groups. A randomized, multicenter NUTRIREA-2 study was carried out by Reignier, et al. [14] showed that there was no significant difference in the comparison of ICU acquired infections, ventilator-associated pneumonia, bacteremia and urinary infections between the EN and the PN groups. The study of Blaser, et al. [15] revealed that the risk of infection was significantly lower in the EN group between the ICU patients who received early EN or PN. In our study, nosocomial infections (65.5%), the presence of infection (74.5%) and sepsis (61.8%) were significantly higher in the EN group.
In the study on 185 patients, 89 of whom received enteral nutrition and 96 received parenteral nutrition, Tao, et al. [13] revealed significantly higher mortality rates among the PN group. Yan, et al. [16] noted no significant difference in mortality rate between the EN and PN groups. In the NUTRIREA-2 study carried out by Reignier, et al. [14], there was no significant difference in 28-day mortality between two groups. Our study revealed that 28-day mortality was higher in the PN group (28.9%) compared to the EN group (23.6%); however, no statistically significant difference was noted between the two groups.
Tao, et al. [13] and Yan, et al. [16] found that the length of hospital stay was statistically shorter in patients who received enteral nutrition. Grau, et al. [12] stated that the length of stay in ICU and on MV was statistically higher in the group who received enteral nutrition. In our study, the length of stay in ICU and the length of stay on MV were higher in the EN group, and this supports the study conducted by Grau, et al. [12]. We consider that this situation resulted from the fact that the patients receiving enteral nutrition were followed-up mostly due to medical reasons rather than surgical reasons, and this lead in a more extended stay in the ICU and on the MV. We think that the fact that the length of stay in the ICU and on the MV is shorter among parenterally fed patients is mostly due to the frequent surgical follow-ups, which is associated with lower incidence rates of nosocomial infections, presence of infection and sepsis development.
The study of Isil, et al. [17] on 152 patients, where they performed an annual nutrition review, they found that 2.6% of the patients receiving PN developed central venous catheter obstruction and 0.7% developed pneumothorax. In our study, of 45 patients receiving PN, 13.3% showed mechanical complications, 2.2% developed pneumothorax, 2.2% showed arterial puncture, 4.4% developed abscess/hematoma and 4.4% developed catheter obstruction.
The studies demonstrated that enteral nutrition may lead to metabolic, gastrointestinal and mechanical complications. The possible mechanical complications include malposition, tube occlusion and pulmonary aspiration leading to death [18]. In our study, 21.8% of 55 patients in the EN group developed mechanical complications, 9.1% were due to aspiration pneumonia and 18.2% were due to tube occlusion.
The study carried out by Harvey, et al. [11] demonstrated that the rate of hypoglycemia was significantly lower in the group that received parenteral nutrition compared to the group that received enteral nutrition. In the study carried out by Tao, et al. [13], hyperglycemia was observed in 32 from 96 patients who received parenteral nutrition; while it was observed in 18 from 80 patients who received enteral nutrition. However, there was found no statistically significant difference. In a randomized study carried out by Moore Fa, et al [19], it was determined that blood glucose levels were higher in the patient group who received parenteral nutrition compared to patients who received enteral nutrition. In our study, hyperglycemia was observed in 74.5% of the patients who receive EN and hypoglycemia was noted in 32.7% of the patients. Hyperglycemia was observed in 66.7% of the patients receiving PN, and hypoglycemia was detected in 31.1%. There was no significant difference in terms of hyperglycemia and hypoglycemia between the two groups. There was no significant difference in hypernatremia and hypophosphatemia between two groups in our study. Similar to our study, Harvey, et al. [11] reported no significant difference in electrolyte disturbances.
Hepatic dysfunction is a gastrointestinal complication, such as PN-associated steatosis, cholestasis and gallstones and it has a higher prevalence in patients who receive long-term PN. At the same time, it is known that parenteral nutrition may lead to changes in serum transaminase, ALP and bilirubin [18]. The study of Grau, et al [12] noted that 30% of the patients who receive PN developed hepatic dysfunction. In parallel to this study, 28.9% of the patients who receive PN developed hepatic dysfunction in our study.
The study carried out by Park, et al. [20] including early enteral and parenteral feeding in patients with pancreaticoduodenectomy noted that 5.5% of the patients who receive enteral nutrition developed vomiting, 5.5% showed diarrhoea and 5.5% had nausea. In the study was carried out by Reignier, et al. [14], 34% of the patients who receive enteral nutrition showed nausea and 36% showed diarrhea. In our study, 49.1% of the patients who receive enteral nutrition had nausea, 32.7% developed vomiting, 36.4% developed diarrhoea and 67.3% developed constipation. We presume that the high rates are caused by the longer length of hospital stay in the EN group.
In their study that they evaluated the complications and contributing factors in the patients who receive enteral pump feeding in ICU, Metin, et al. [21] noted that 72.5% of the patients were fed by nasogastric tube and 27.7% were fed by PEG tube. In our study, 87.3% of the patients were fed by nasogastric tubes and 12.7% were fed by percutaneous tubes (PEG/PEJ).
The study of Harvey, et al. [11] revealed that there was no statistically significant difference between the APACHE II scores and 30-day mortality in the EN and PN groups. Blaser, et al. [15] noted no significant difference in mortality in the comparison between the patients receiving early EN and early PN in the ESICM clinical practice guidelines regarding early enteral nutrition in ICU patients. In the study carried out by Tao, et al. [13], there was no significant difference in the APACHE II scores between the EN and PN groups. Although the mean APACHE II score and 28-day mortality were higher in the PN group, no statistically significant difference was found between the two groups in our study.
The retrospective structure of our study was limited in some aspects; however, we tried to compare the complications associated with enteral and parenteral nutrition in intensive care patients with similar demographic characteristics. In our study, there was no statistically significant difference between the two groups although the PN group had a higher mortality rate. Nosocomial infection rates, the incidence rate of infection and sepsis development were higher in the patients who received enteral nutrition. We consider that the high rates are associated with the fact that the patients receiving enteral nutrition have medical conditions, which result in an extended stay in the ICU and on the MV. On the other hand, the length of stay in ICU and the length of stay on MV are relatively shorter in patients who receive parenteral nutrition as the reason for admission is mostly surgery. Therefore, nosocomial infections, the presence of infection and sepsis development are lower in the PN group.
There are some limitations of this study. First, this is a retrospective study not a prospective. Second, the sample sizes of our groups are a bit small. We need more prospective randomized studies on multicenter design in large groups.
In conclusion, we presume that the length of stay in ICU and the reason for admission play a more crucial role in the development of infection and mortality rather than enteral or parenteral nutrition. Further studies with a prospective randomized clinical trial design are required for clarifying on this topic.
- ASPEN Board of Directors and the Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr. 2002; 26: 1SA-138SA. PubMed: https://pubmed.ncbi.nlm.nih.gov/11841046/
- Tamiya H, Yasunaga H, Matusi H, Fushimi K, Akishita M, et al. Comparison of short-term mortality and morbidity between parenteral and enteral nutrition for adults without cancer: a propensity-matched analysisi using a national inpatient database. Am J Clin Nutr. 2015; 102: 1222-1228. PubMed: https://pubmed.ncbi.nlm.nih.gov/26447149/
- Eroglu A. The effect of intravenous alanyl-glutamine supplementation on plasma glutathione levels in intensive care unit trauma patients receiving enteral nutrition: the results of a randomized controlled trial. Anesth Analg. 2009; 109: 502-505. PubMed: https://pubmed.ncbi.nlm.nih.gov/19608826/
- Moore FA, Feliciano DV, Andrassy RJ, McArdle AH, Booth FV, et al. Early enteral feeding, compared with parenteral reduces postoperative septic complications. Ann. Surg. 1992; 190:172-182. PubMed: https://pubmed.ncbi.nlm.nih.gov/1386982/
- Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019; 38: 48-79. PubMed: https://pubmed.ncbi.nlm.nih.gov/30348463/
- Taylor BE, McClave SA, Martindale RG, Warren MM, Johnson DR, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Crit Care Med. 2016; 44: 390-438. PubMed: https://pubmed.ncbi.nlm.nih.gov/26771786/
- Heidegger CP, Darmon P, Pichard C. Enteral vs. parenteral nutrition for the critically ill patient: a combined support should be preferred. Current Opin Crit Care. 2008; 14: 408-414. PubMed: https://pubmed.ncbi.nlm.nih.gov/18614904/
- Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P. Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. J Parenteral Enteral Nutr. 2003. 27: 355-373. PubMed: https://pubmed.ncbi.nlm.nih.gov/12971736/
- Zaloga GP. Parenteral nutrition in adult inpatients with functioning gastrointestinal tracts: assessment of outcomes. Lancet. 2006; 367: 1101-1111. PubMed: https://pubmed.ncbi.nlm.nih.gov/16581410/
- Liu CL, Du Z, Lou C, Wu C, Yuan Q, et al. Enteral nutrition is superior to total parenteral nutrition for pancreatic cancer patients who underwent pancreaticoduodenectomy. Asia Pacific J Clin Nutr. 2011; 20.2: 154-160. PubMed: https://pubmed.ncbi.nlm.nih.gov/21669582/
- Harvey SE, Parrott F, Harrison DA, Bear DE, Segaran E, et al. Trial of the route of early nutritional support in critically ill adults. N Engl J Med. 2014; 371: 1673-1684. https://pubmed.ncbi.nlm.nih.gov/25271389/
- Grau T, Bonet A, Rubio M, Mateo D, Farré M, et al. Liver dysfunction associated with artificial nutrition in critically ill patients. Critical Care. 2007; 11: R10. PubMed: https://pubmed.ncbi.nlm.nih.gov/17254321/
- Tao Y, Tang C, Feng W, Bao Y, Yu H. Early nasogastric feeding versus parenteral nutrition in severe acute pancreatitis: A retrospective study. Pak J Med Sci. 2016; 32: 1517-1521. PubMed: https://pubmed.ncbi.nlm.nih.gov/28083056/
- Reignier J, Boisramé-Helms J, Brisard L, Lascarrou JB, Ait Hssain A, et al. Enteral versus parenteral early nutrition in ventilated adults with shock: a randomised, controlled, multicentre, open-label, parallel-group study (NUTRIREA-2). The Lancet. 2018; 391: 133-143. PubMed: https://pubmed.ncbi.nlm.nih.gov/29128300/
- Blaser AR, Starkopf J, Alhazzani W, Berger MM, Casaer MP, Deane AM, Fruhwald S, Hiesmayr M, et al. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines. Intensive Care Med. 2007; 43: 380-398. PubMed: https://pubmed.ncbi.nlm.nih.gov/28168570/
- Yan X, Zhou FX, Lan T, Xu H, Yang XX, et al. Optimal postoperative nutrition support for patients with gastrointestinal malignancy: A systematic review and meta-analysis. Clinical Nutrition. 2017; 36: 710-721. PubMed: https://pubmed.ncbi.nlm.nih.gov/27452745/
- Işıl CT, Türk HŞ, Totoz T, Oba S. Reanimasyon ünitemizin bir yıllık nütrisyon profili. Ş.E.E.A.H. Tıp Bülteni. 2013; 47: 147-150.
- Cotogni P. Management of parenteral nutrition in critically ill patients. World J Crit Care Med. 2017; 6: 13-20. PubMed: https://pubmed.ncbi.nlm.nih.gov/28224103/
- Moore FA, Moore EE, Jones TN, McCroskey BL, Peterson VM. TEN versus TPN following major abdominal trauma-reduced septic morbidity. J Trauma. 1989; 29: 916–923. PubMed: https://pubmed.ncbi.nlm.nih.gov/2501509
- Park JS, Chung HK, Hwang HK, Kim JK, Yoon DS. et al. Postoperative nutritional effects of early enteral feeding compared with total parental nutrition in pancreaticoduodectomy patients: a prosepective, randomized study. J Korean Med Sci. 2012; 27: 261-267. PubMed: https://pubmed.ncbi.nlm.nih.gov/22379336/
- Metin ZG, Özdemir L. Yoğun Bakımda Enteral Pompa ile Beslenen Hastalarda Gelişen Komplikasyonlar ve Etkileyen Faktörlerin Belirlenmesi. Hacettepe Üniversitesi Hemşirelik Fakültesi Dergisi. 2015; 2: 20–29.